Rev’s Transcript Library
Explore our extensive collection of free transcripts from political figures and public events. Journalists, students, researchers, and the general public can explore transcripts of speeches, debates, congressional hearings, press conferences, interviews, podcasts, and more.

Super Bowl Post Press Conference
Super Bowl MVP Kenneth Walker III and Seahawks’ head coach Mike Macdonald speak following Super Bowl LX. Read the transcript here.

DOJ Press Conference on 2/06/26
The Department of Justice says the FBI has arrested a participant in the 2012 Benghazi attack. Read the transcript here.
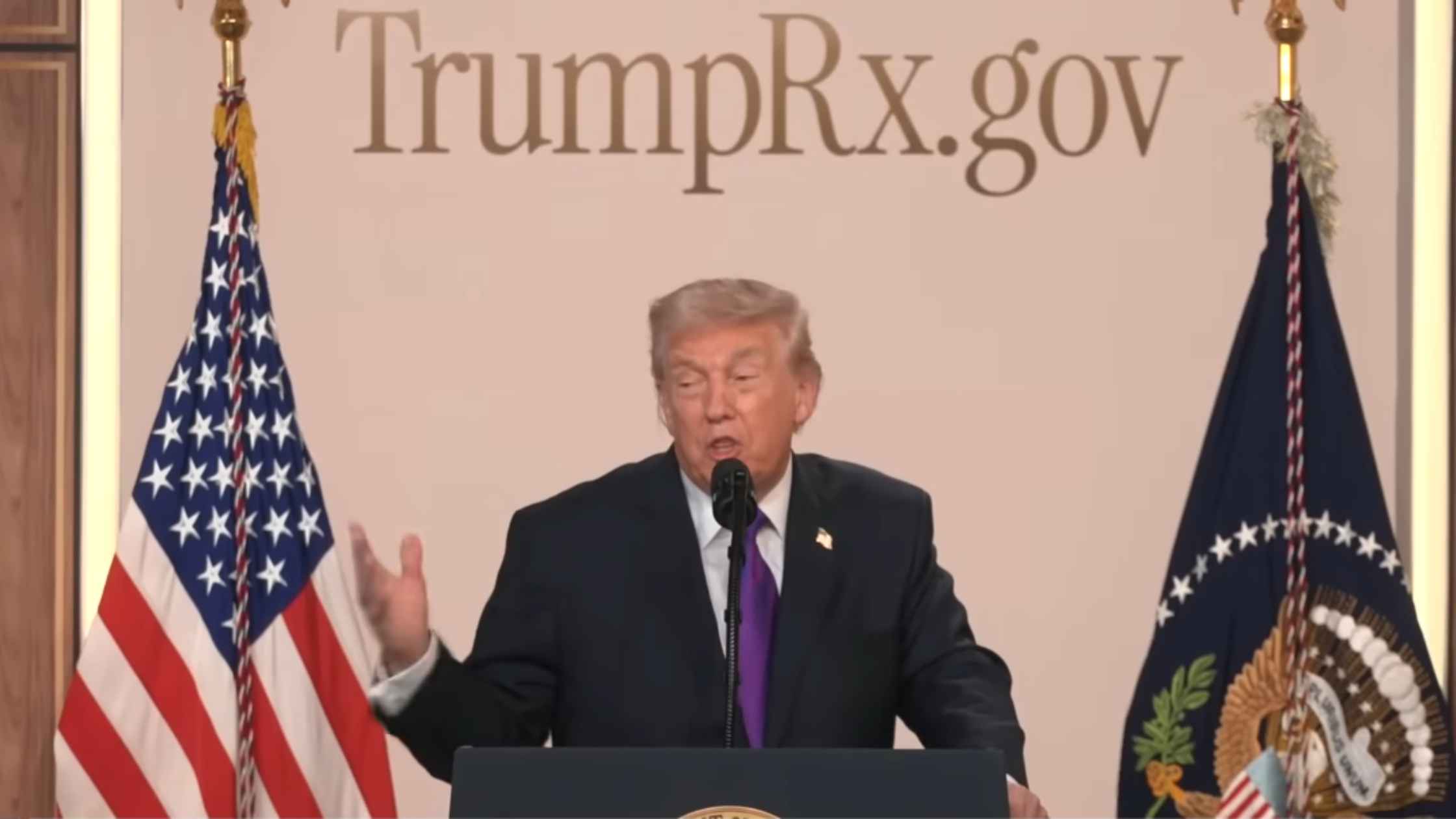
TrumpRX Announcement
Donald Trump announces the opening of the TrumpRX website. Read the transcript here.
Karoline Leavitt White House Press Briefing on 2/05/26
Karoline Leavitt holds the White House Press Briefing for 2/05/26. Read the transcript here.
National Prayer Breakfast
Donald Trump speaks at the National Prayer Breakfast. Read the transcript here.

Human Rights Watch Annual World Report
Human Rights Watch releases its annual World Report documenting the state of human rights in more than 100 countries. Read the transcript here.

Border Wall Press Conference
Secretary of Homeland Defense Kristi Noem provides an update on the border wall. Read the transcript here.

Homan News Conference in Minneapolis
Tom Homan announces the withdrawal of 700 federal officers from Minnesota. Read the transcript here.
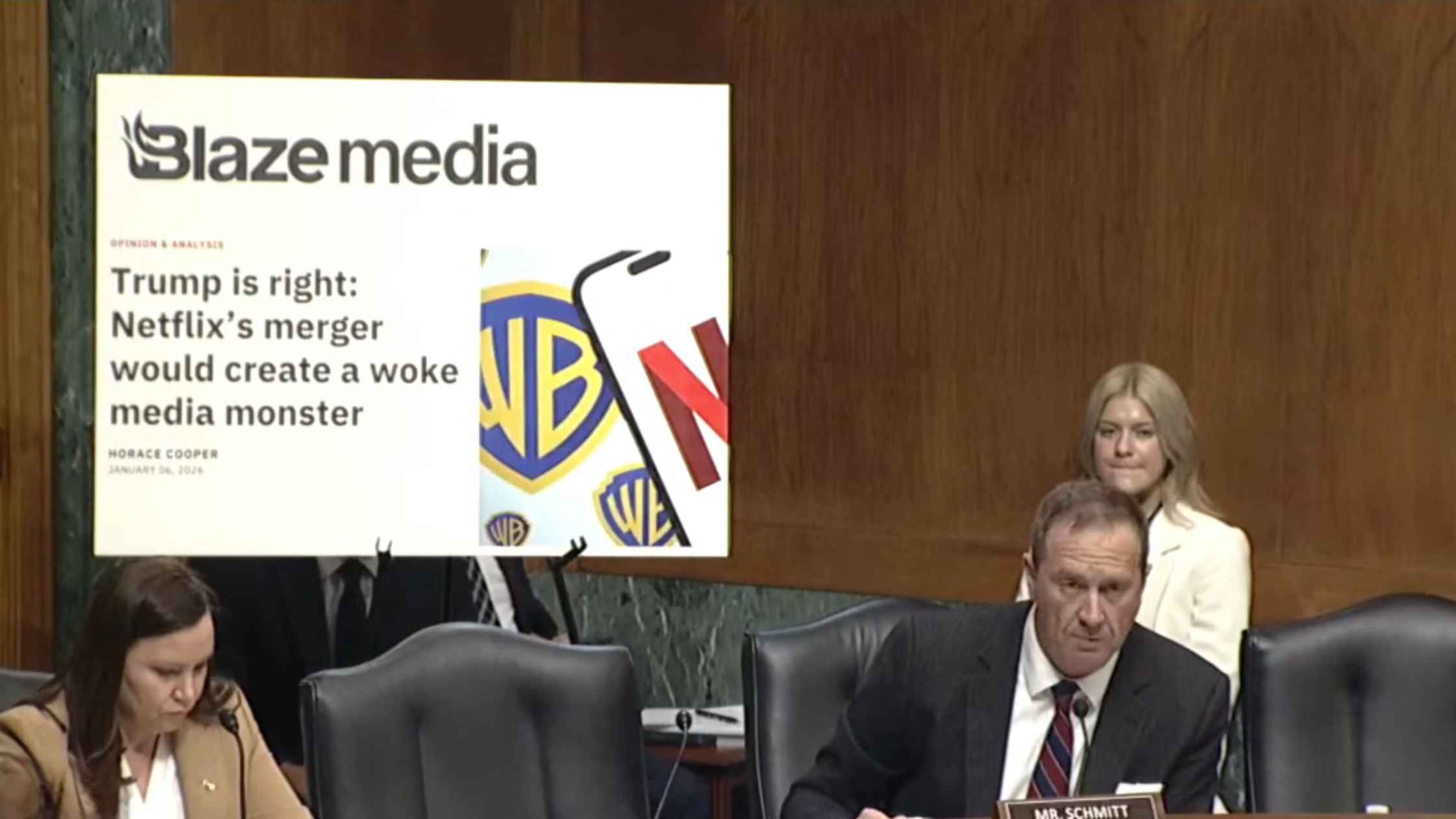
Netflix-Warner Brothers Merger Hearing
Senate Judiciary hearing examines proposed Netflix-Warner Brothers deal. Read the transcript here.
Subscribe to The Rev Blog
Sign up to get Rev content delivered straight to your inbox.








