Rev’s Transcript Library
Explore our extensive collection of free transcripts from political figures and public events. Journalists, students, researchers, and the general public can explore transcripts of speeches, debates, congressional hearings, press conferences, interviews, podcasts, and more.

Ilhan Omar Accosted at Town Hall
Ilhan Omar was shouted at and had liquid sprayed on her by an individual at a town hall in Minneapolis. Read the transcript here.

Arizona Shooting Press Conference
Pima County Sheriff holds a press conference on Arizona Border Patrol shooting. Read the transcript here.
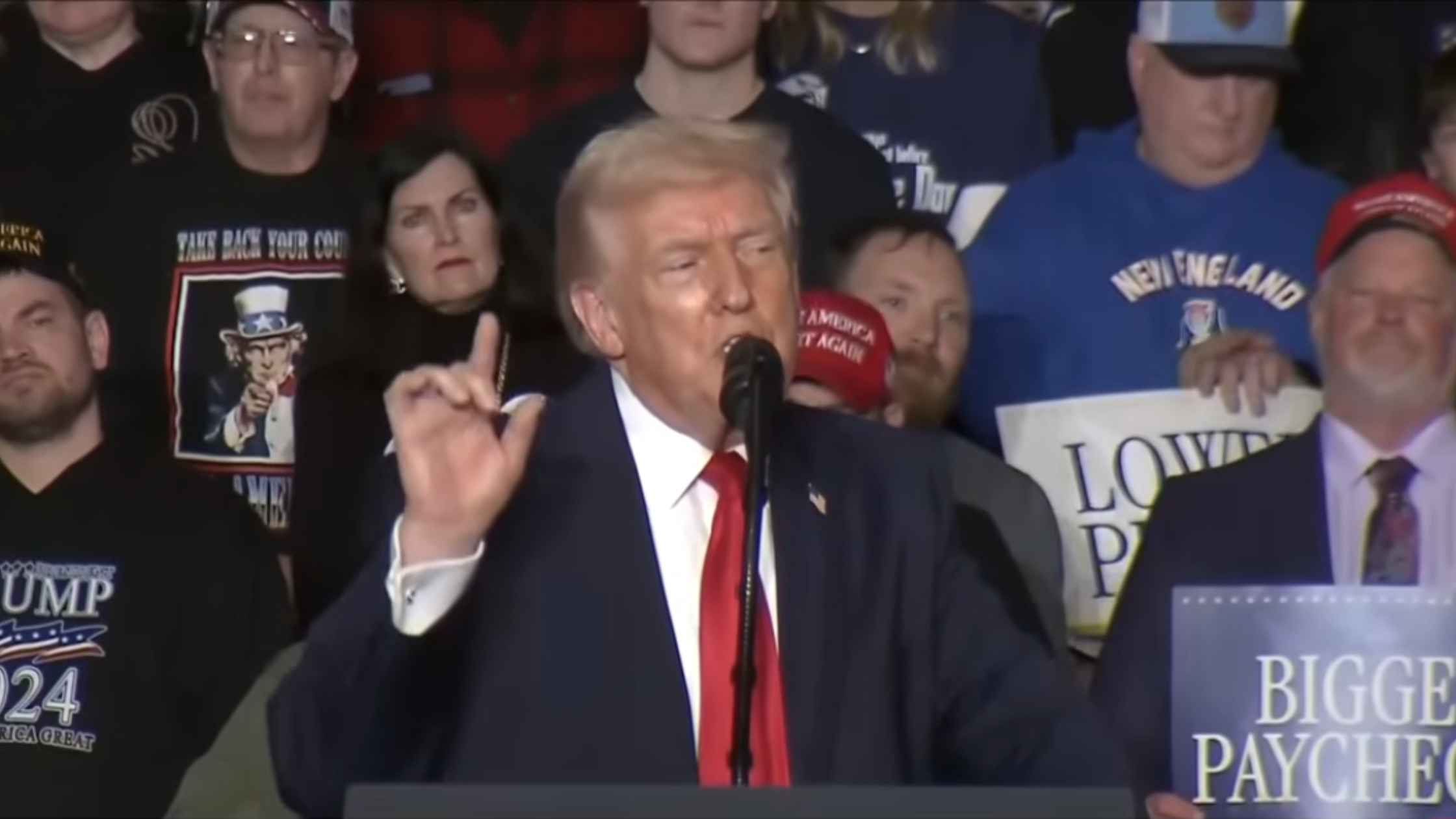
Trump Remarks in Iowa 1/27/26
Donald Trump delivers remarks on the economy in Clive, Iowa on 1/27/26. Read the transcript here.
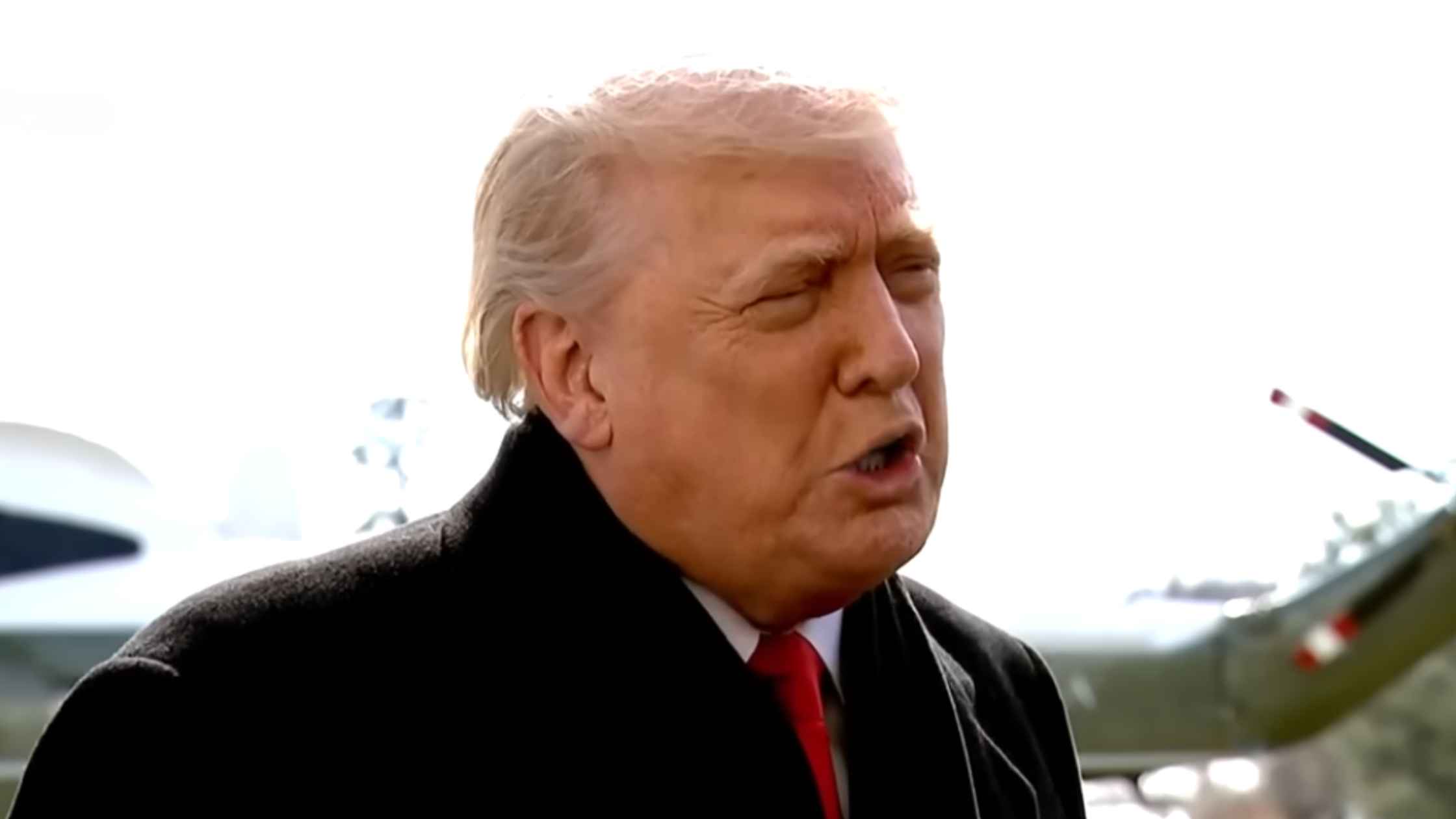
Trump Press Gaggle 1/27/26
Donald Trump speaks with reporters on 1/27/26 outside of the White House before leaving for Iowa. Reads the transcript here.

EU-India Bilateral Summit
Ursula von der Leyen, Antonio Costa, and Narendra Modi deliver remarks during an EU-India bilateral summit. Read the transcript here.
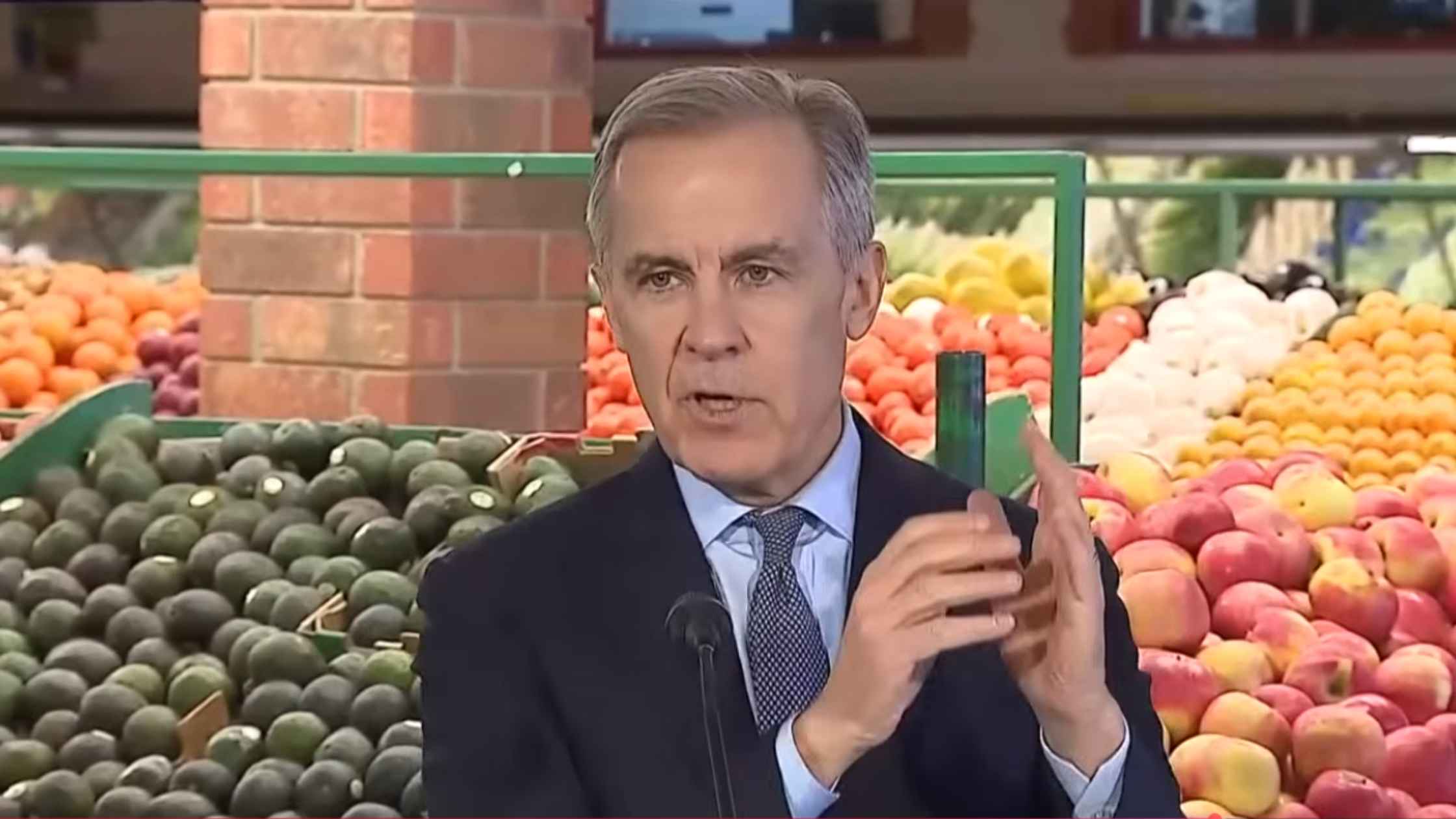
Carney Press Conference
Mark Carney announces "Canada Groceries and Essentials Benefit" to provide support to Canadians facing affordability challenges. Read the transcript here.
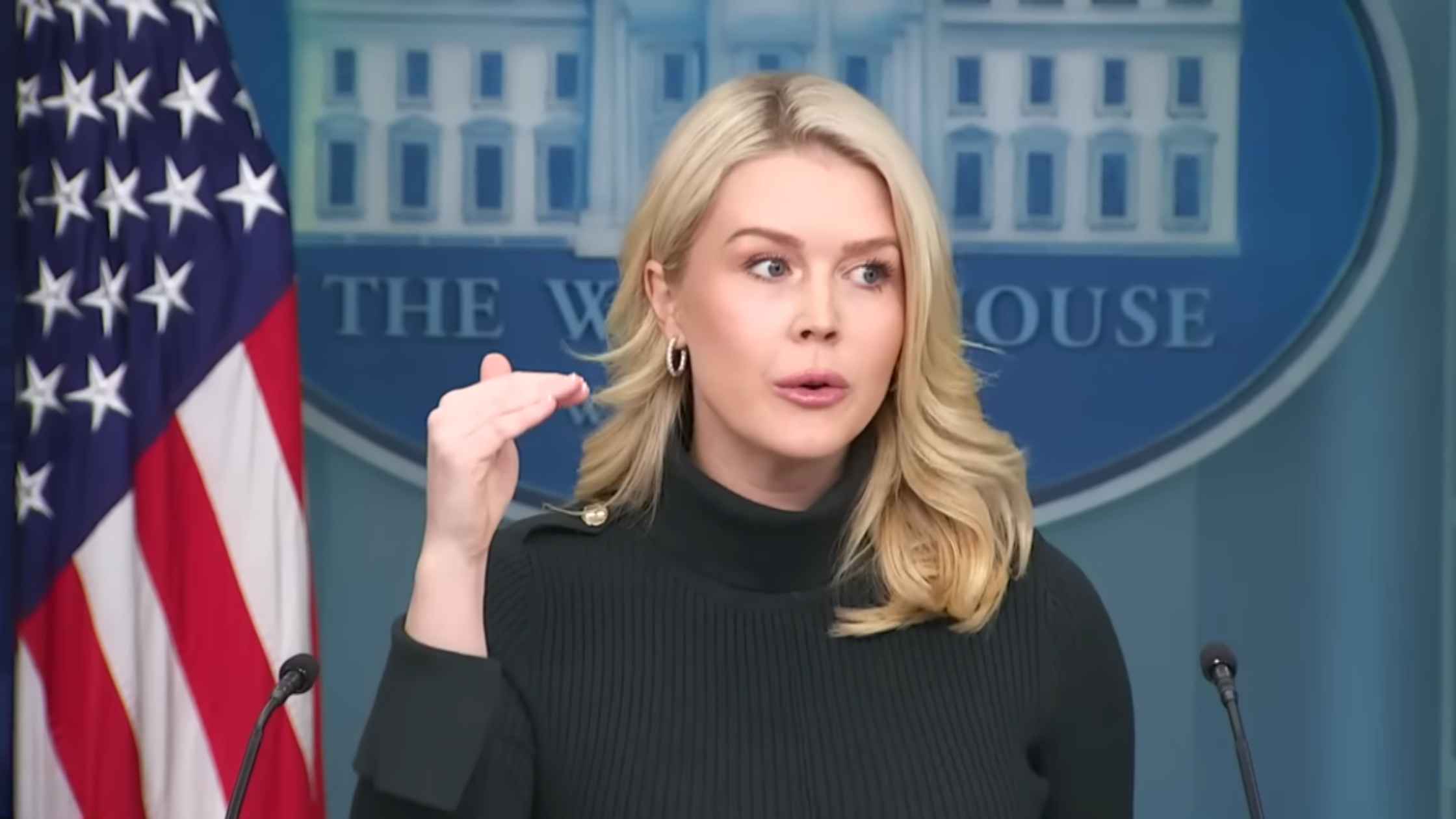
Karoline Leavitt White House Press Briefing on 01/26/26
Karoline Leavitt holds the White House Press Briefing for 01/26/26. Read the transcript here.

Jack Smith Congressional Testimony
Jack Smith testifies publicly before the House Judiciary Committee. Read the transcript here.

Zelenskyy at WEF
Ukrainian President Volodymyr Zelenskyy delivers a special address at the 2026 World Economic Forum in Davos, Switzerland. Read the transcript here.
Subscribe to The Rev Blog
Sign up to get Rev content delivered straight to your inbox.








