Rev’s Transcript Library
Explore our extensive collection of free transcripts from political figures and public events. Journalists, students, researchers, and the general public can explore transcripts of speeches, debates, congressional hearings, press conferences, interviews, podcasts, and more.

United Nations Human Rights Council
The United Nations Human Rights Council starts in Geneva. Read the transcript here.
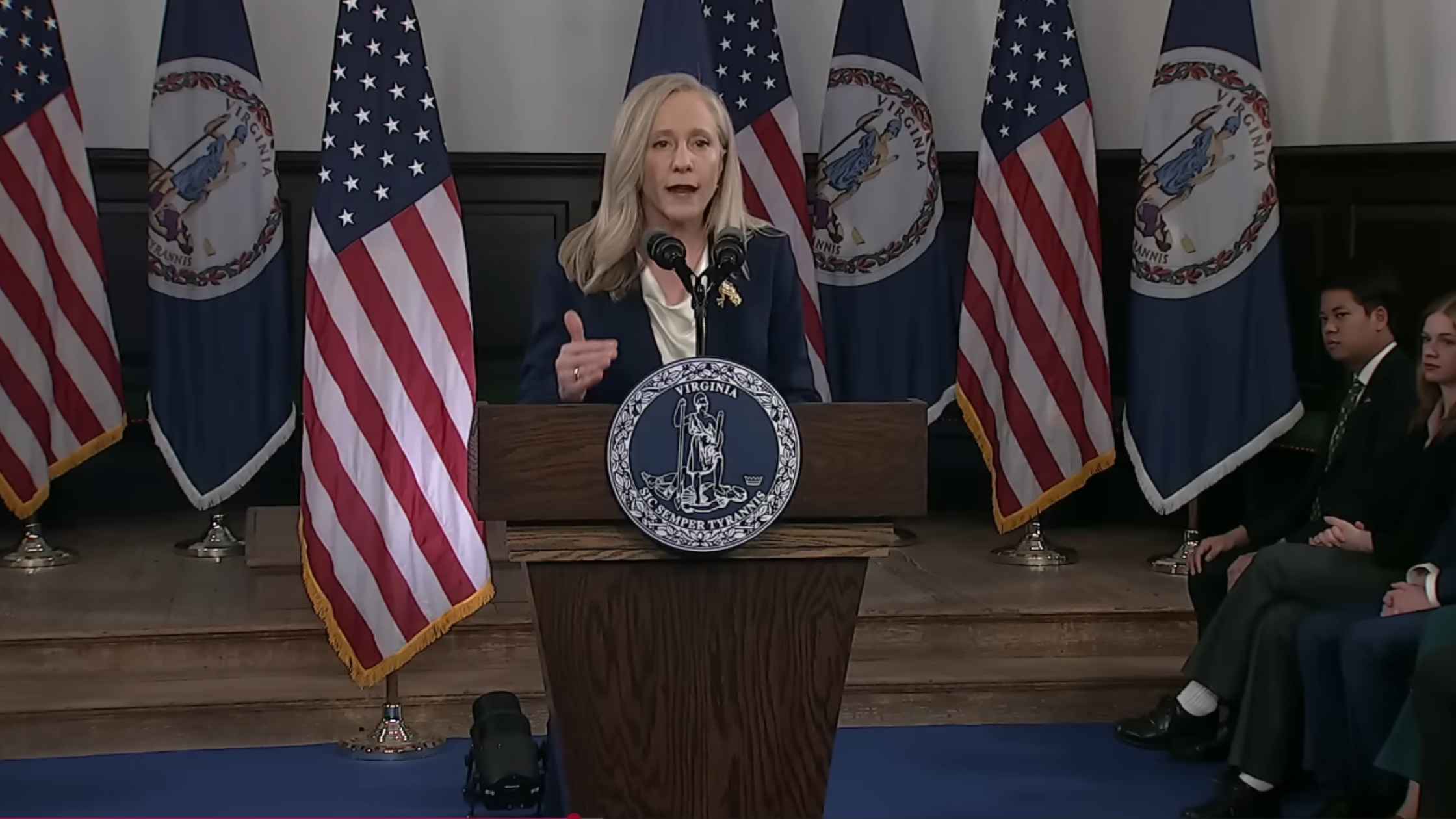
Democrat Response to the 2026 State of the Union Address
Governor Abigail Spanberger delivers the Democratic response to President Trump's State of the Union address. Read the transcript here.

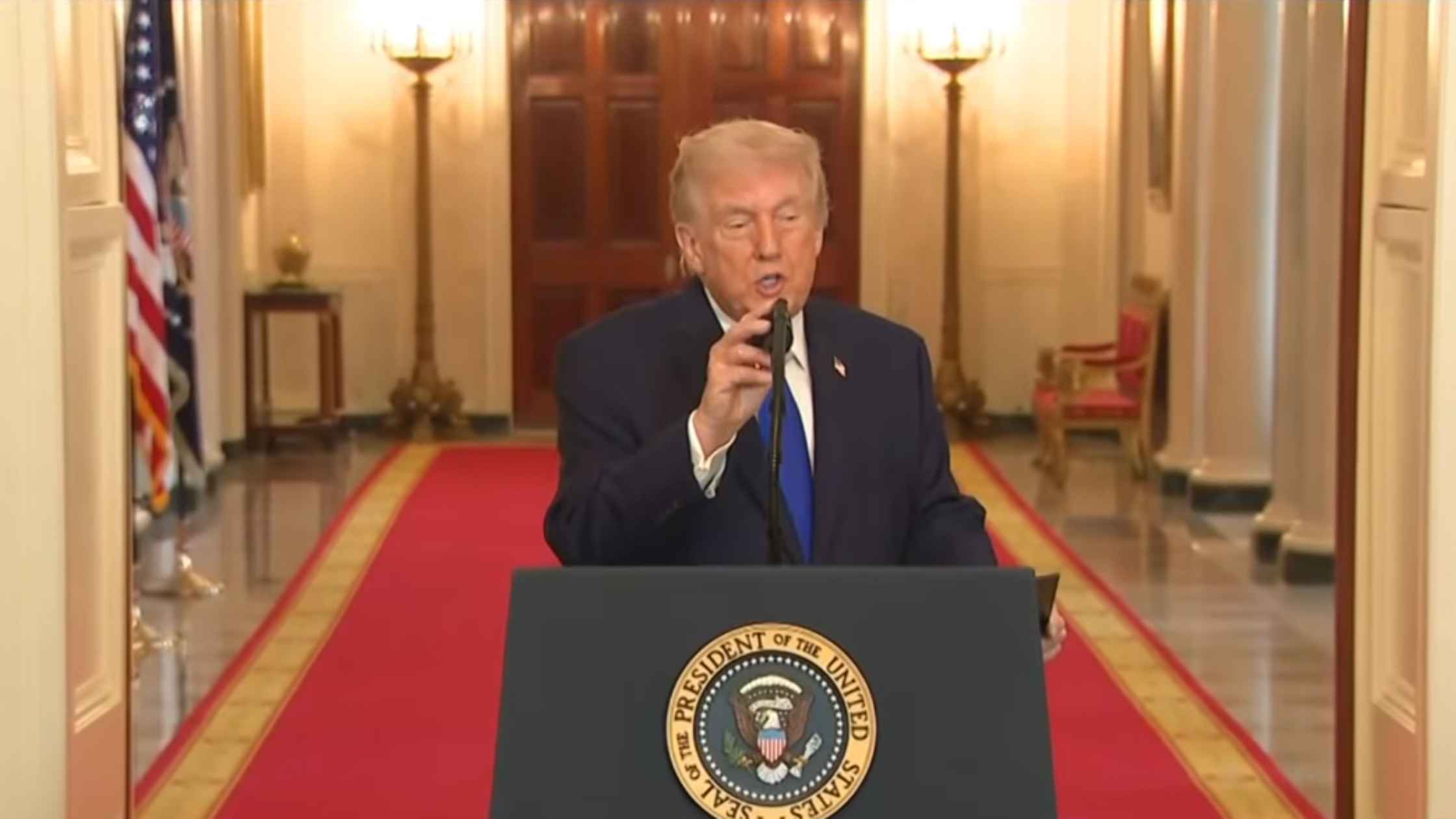
2026 State of the Union Address
U.S. President Donald Trump delivers the 2026 State of the Union address. Read the transcript here.

Home Appliance Hearing
The House Rules Committee holds a hearing on the Home Appliance Protection and Affordability Act and the Homeowner Energy Freedom Act. Read the transcript here.
ICE Whistleblower Hearing
Congressional Democrats hold a public forum to hear testimony from an ICE whistleblower and others. Read the transcript here.
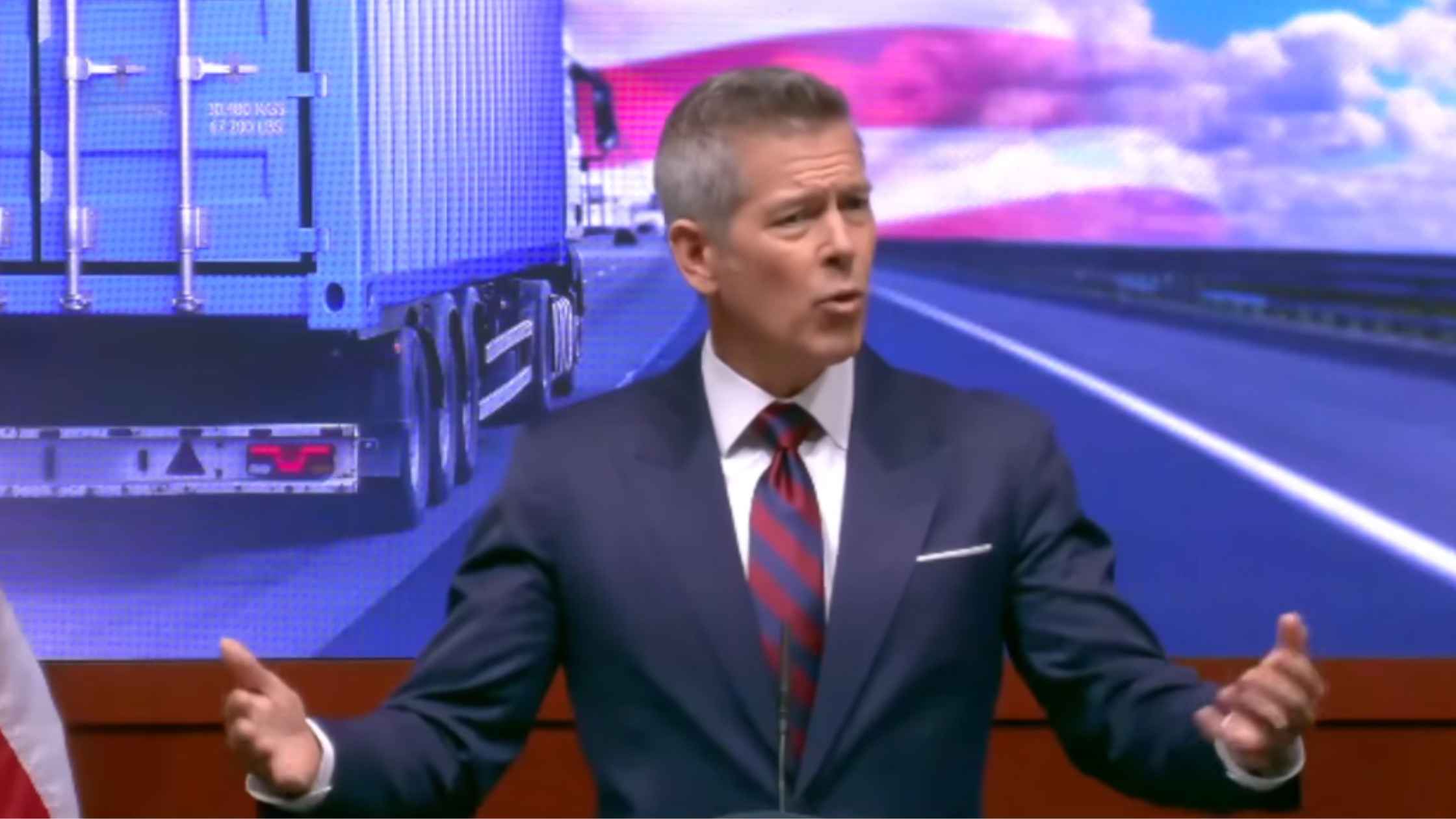
DOT Safety Changes
Secretary of Transportation Sean Duffy announces new DOT Commercial Trucking safety efforts. Read the transcript here.

Bessent at Economic Club of Dallas
Treasury Secretary Scott Bessent delivers remarks at the Economic Club of Dallas. Read the transcript here.
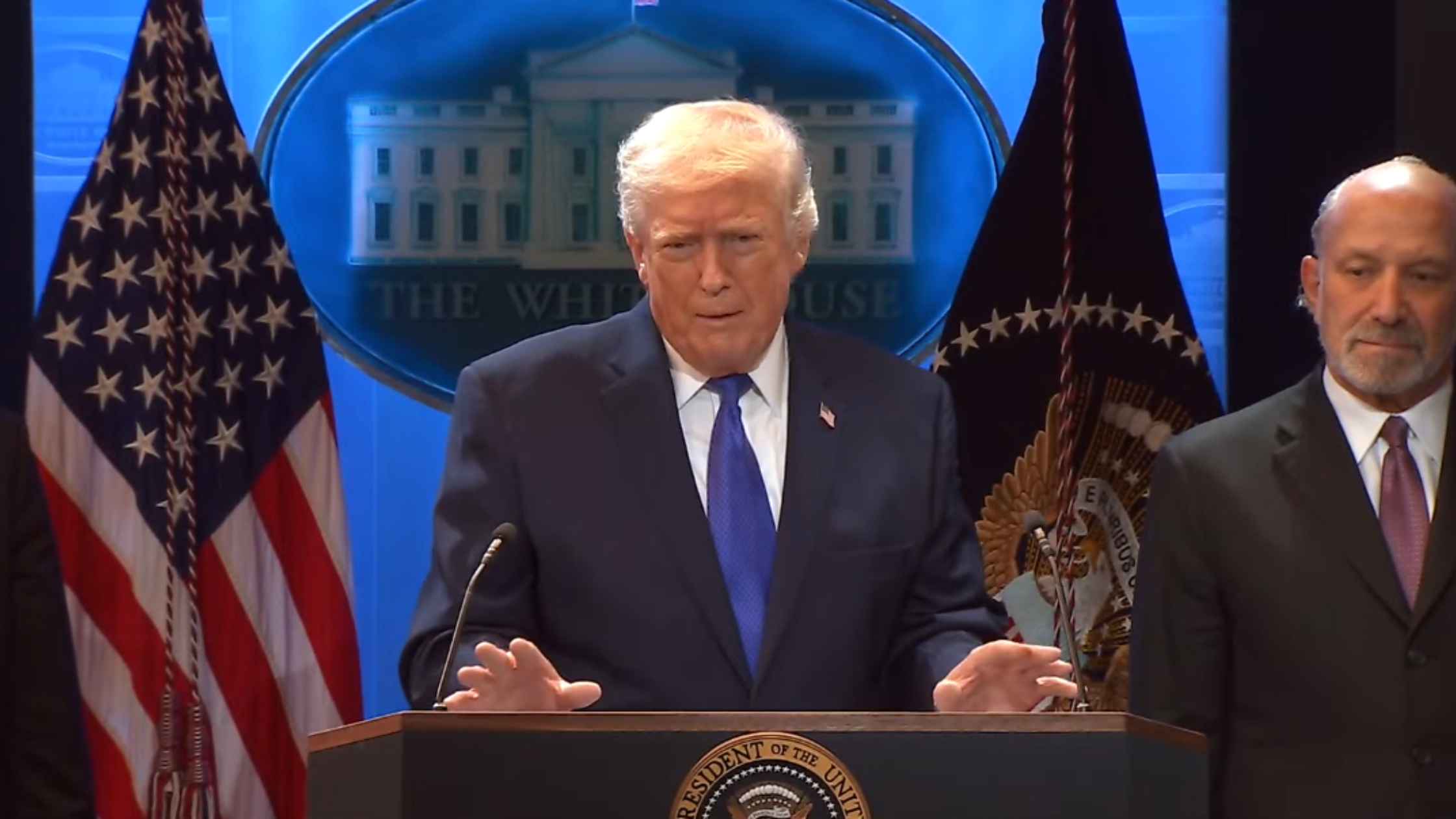
Tariff Ruling Response
Donald Trump responds to the Supreme Court ruling against his tariffs. Read the transcript here.
Subscribe to The Rev Blog
Sign up to get Rev content delivered straight to your inbox.