Rev’s Transcript Library
Explore our extensive collection of free transcripts from political figures and public events. Journalists, students, researchers, and the general public can explore transcripts of speeches, debates, congressional hearings, press conferences, interviews, podcasts, and more.
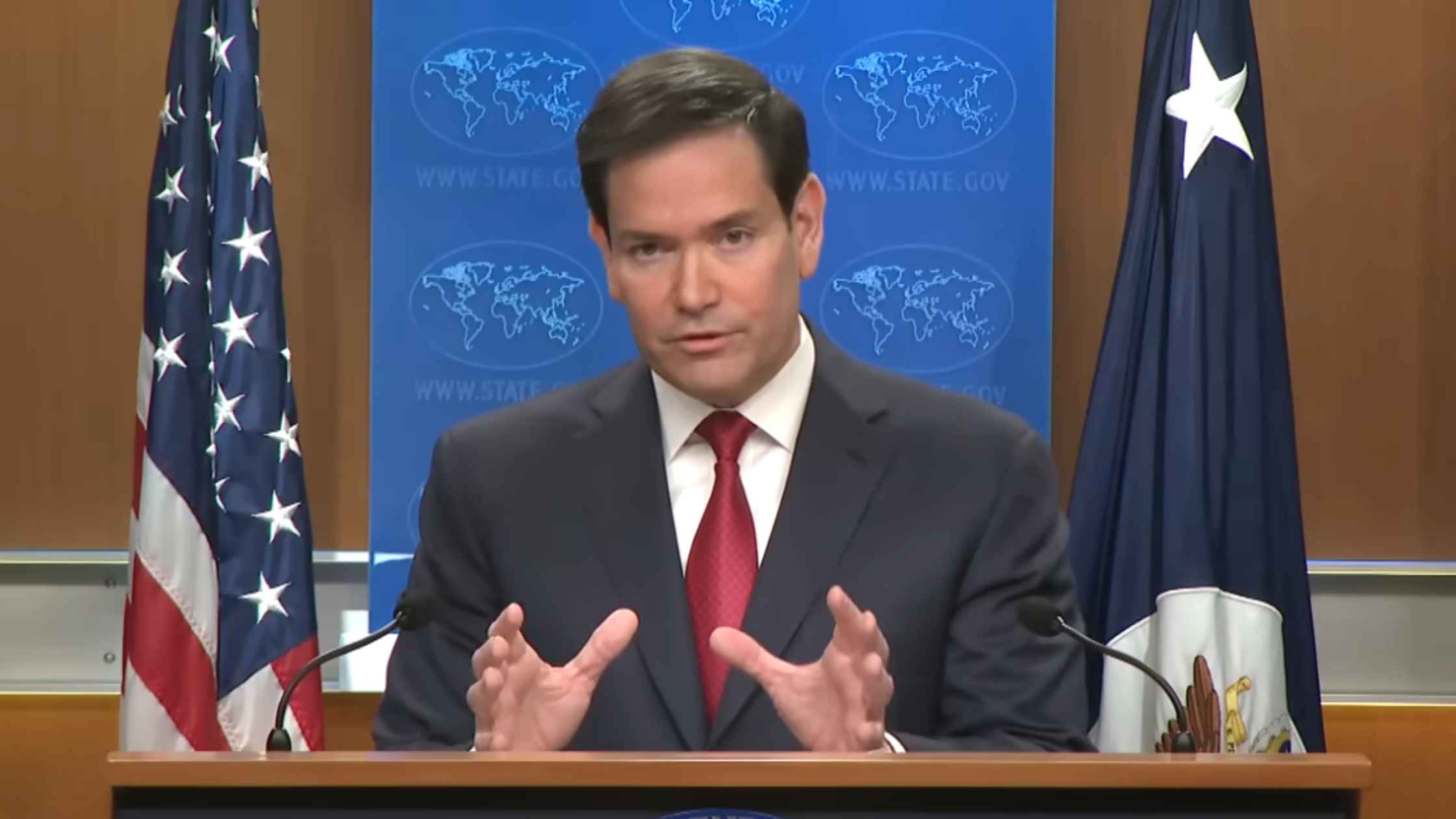
State Department Year End Press Conference
Marco Rubio holds a year-end news conference on Venezuela, the Ukraine War, and Gaza. Read the transcript here.
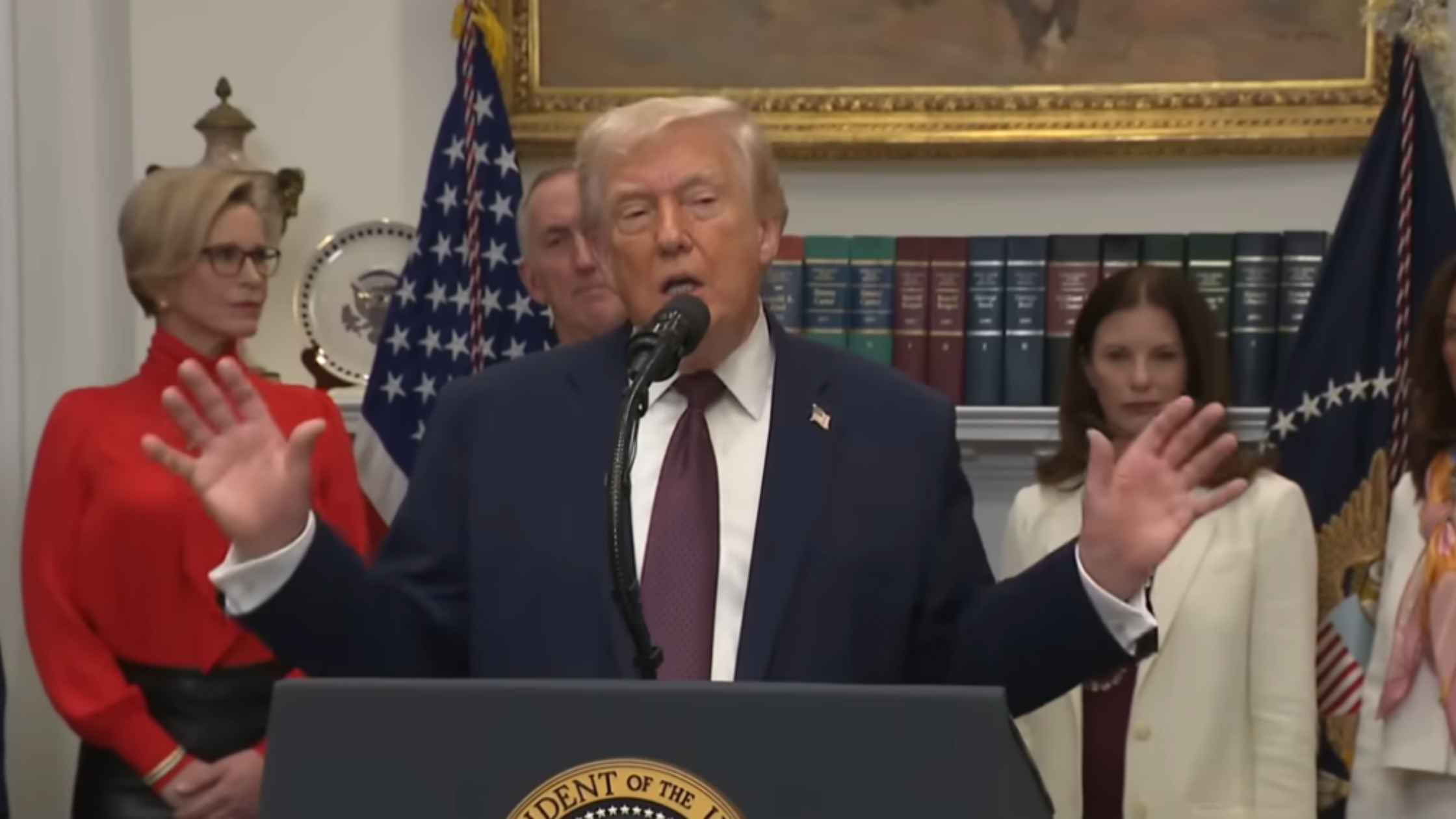
White House Announces Lower Drug Prices
Donald Trump announces "most favored nation" pricing on prescription drugs with major pharmaceutical companies. Read the transcript here.

Joshua vs Paul Post Fight Press Conference
Anthony Joshua vs Jake Paul post-fight press conference. Read the transcript here.
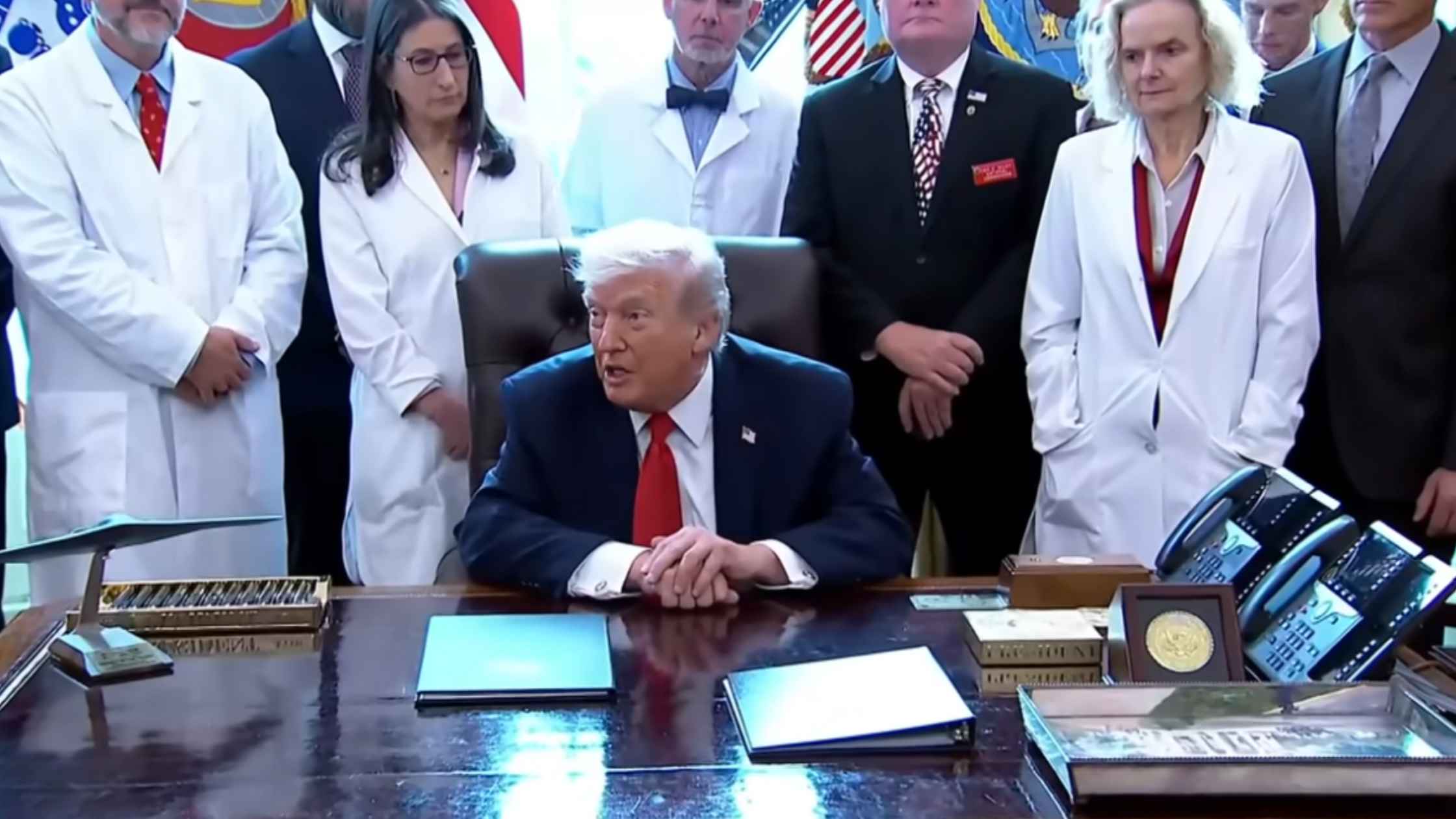
Marijuanna Reclassification
Donald Trump orders the reclassification of marijuana, downgrading it to a Schedule III drug. Read the transcript here.
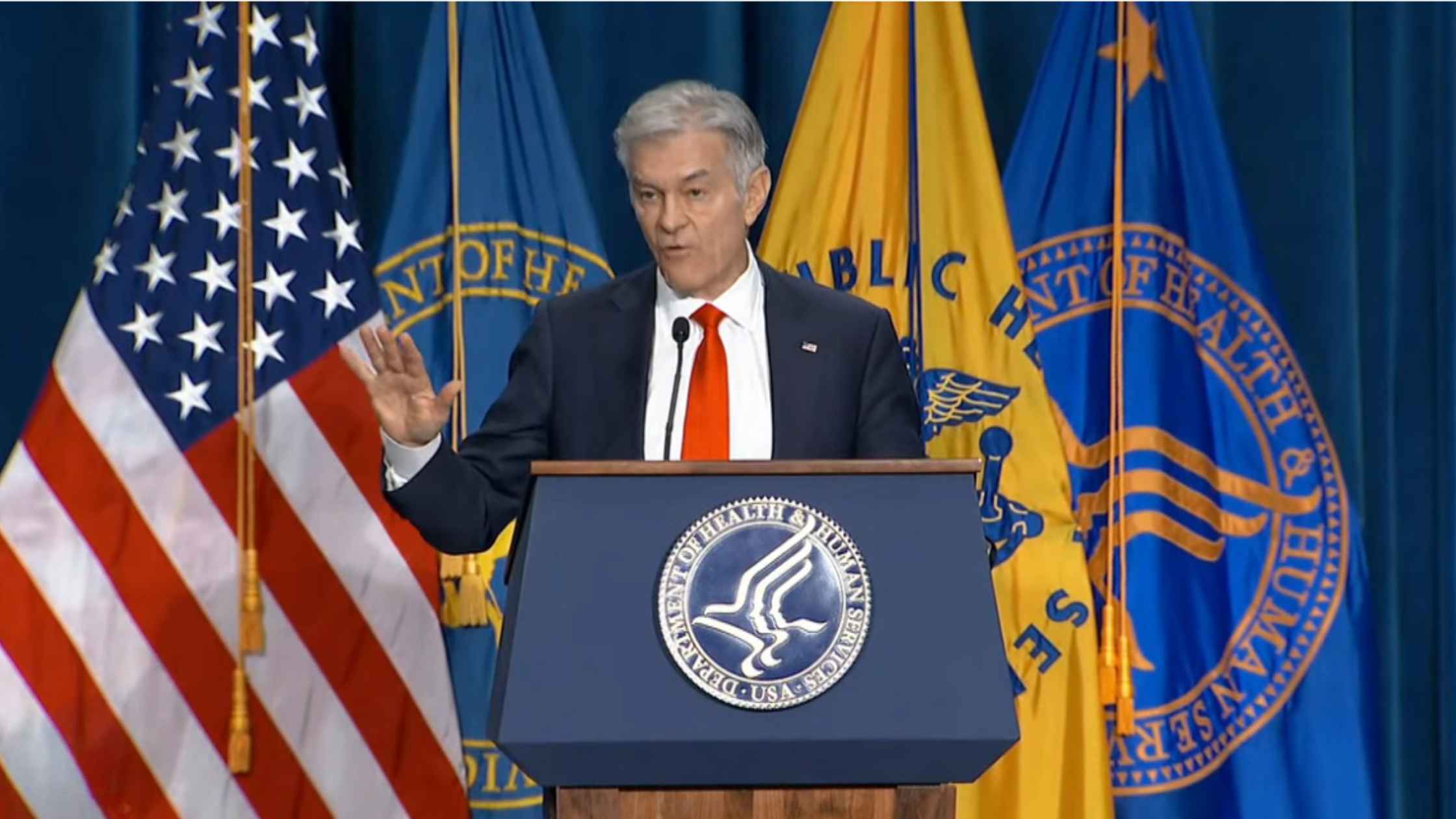
Restrictions On Gender-Affirming Care For Minors
Health Secretary RFK Jr. and Dr. Oz unveil new restrictions on gender identity care for minors. Read the transcript here.

Hearing on Artificial Intelligence
House Homeland Security Committee hearing on artificial intelligence. Read the transcript here.

FCC Oversight Hearing
Senate FCC oversight hearing with FCC chair Brendan Carr. Read the transcript here.
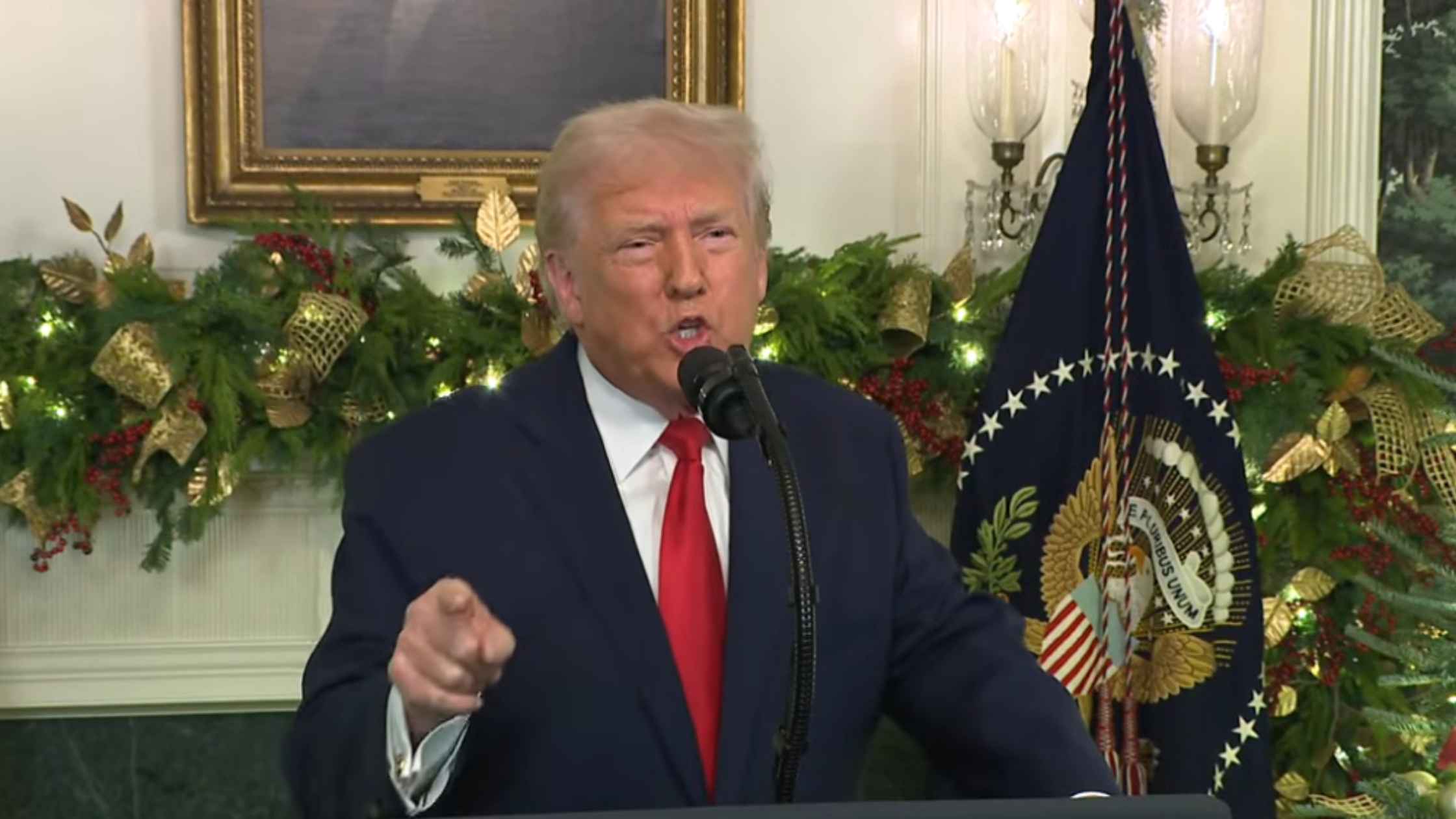
Presidential Address on 12/17/25
Donald Trump gives a Primetime address on 12/17/25. Read the transcript here.

White House Hanukkah Celebration
Donald Trump hosts a Hanukkah celebration at White House. Read the transcript here.
Subscribe to The Rev Blog
Sign up to get Rev content delivered straight to your inbox.








