Rev’s Transcript Library
Explore our extensive collection of free transcripts from political figures and public events. Journalists, students, researchers, and the general public can explore transcripts of speeches, debates, congressional hearings, press conferences, interviews, podcasts, and more.

2026 Oscar Nominations
Danielle Brooks and Lewis Pullman announce the nominations for the 2026 Oscars.
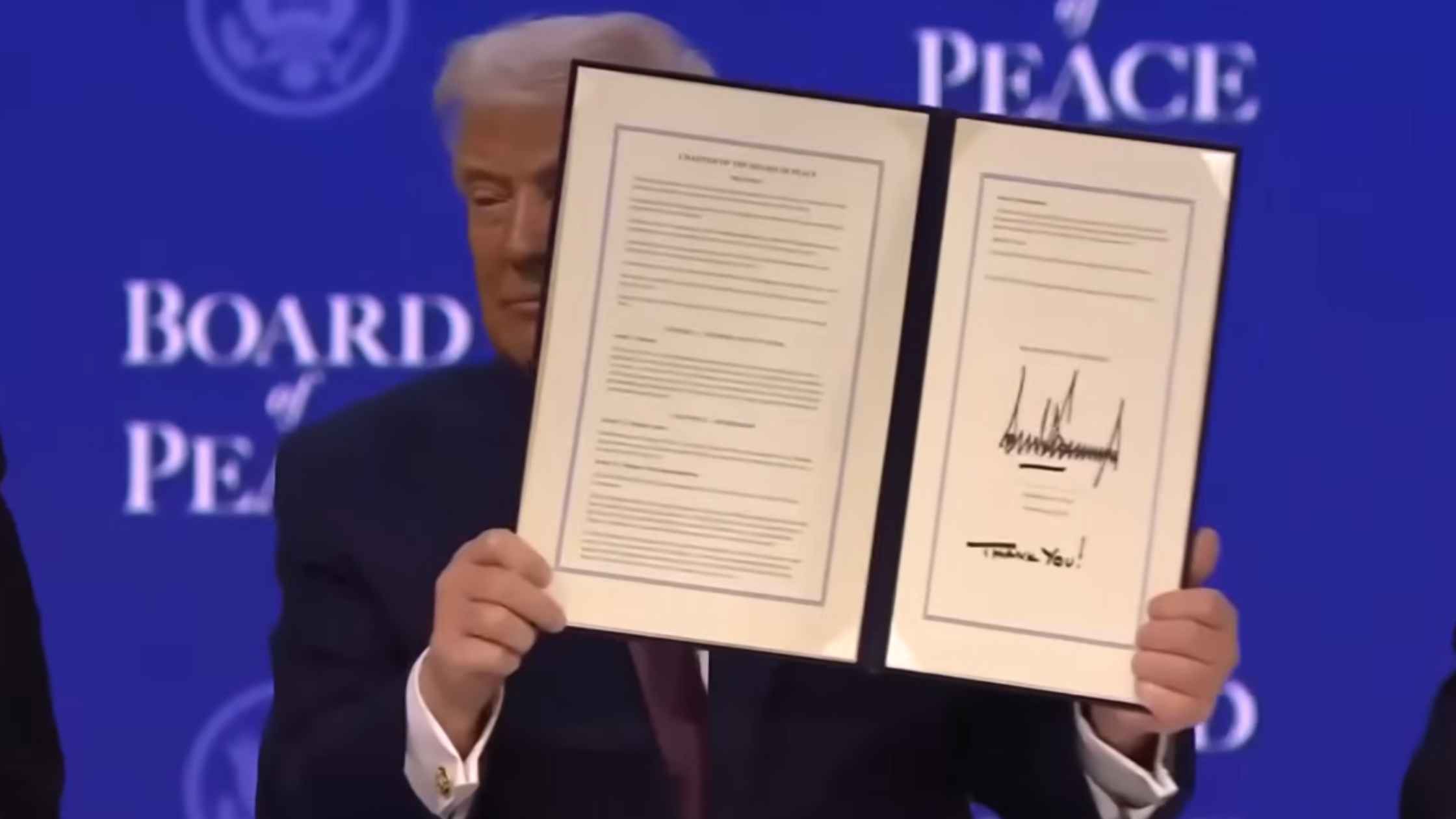
Board of Peace
U.S. President Donald Trump takes part in the Board of Peace charter announcement. Read the transcript here.

Newsom at Davos
California Governor Gavin Newsom speaks at the World Economic Forum in Davos. Read the transcript here.

Merz at Davos
German Chancellor Friedrich Merz gives a special address at the World Economic Forum in Davos. Read the transcript here.

Trump at WEF
Donald Trump speaks at the World Economic Forum annual meeting in Davos. Read the transcript here.

National Archives Preview
The National Archives previews an exhibition marking America's 250th anniversary. Read the transcript here.
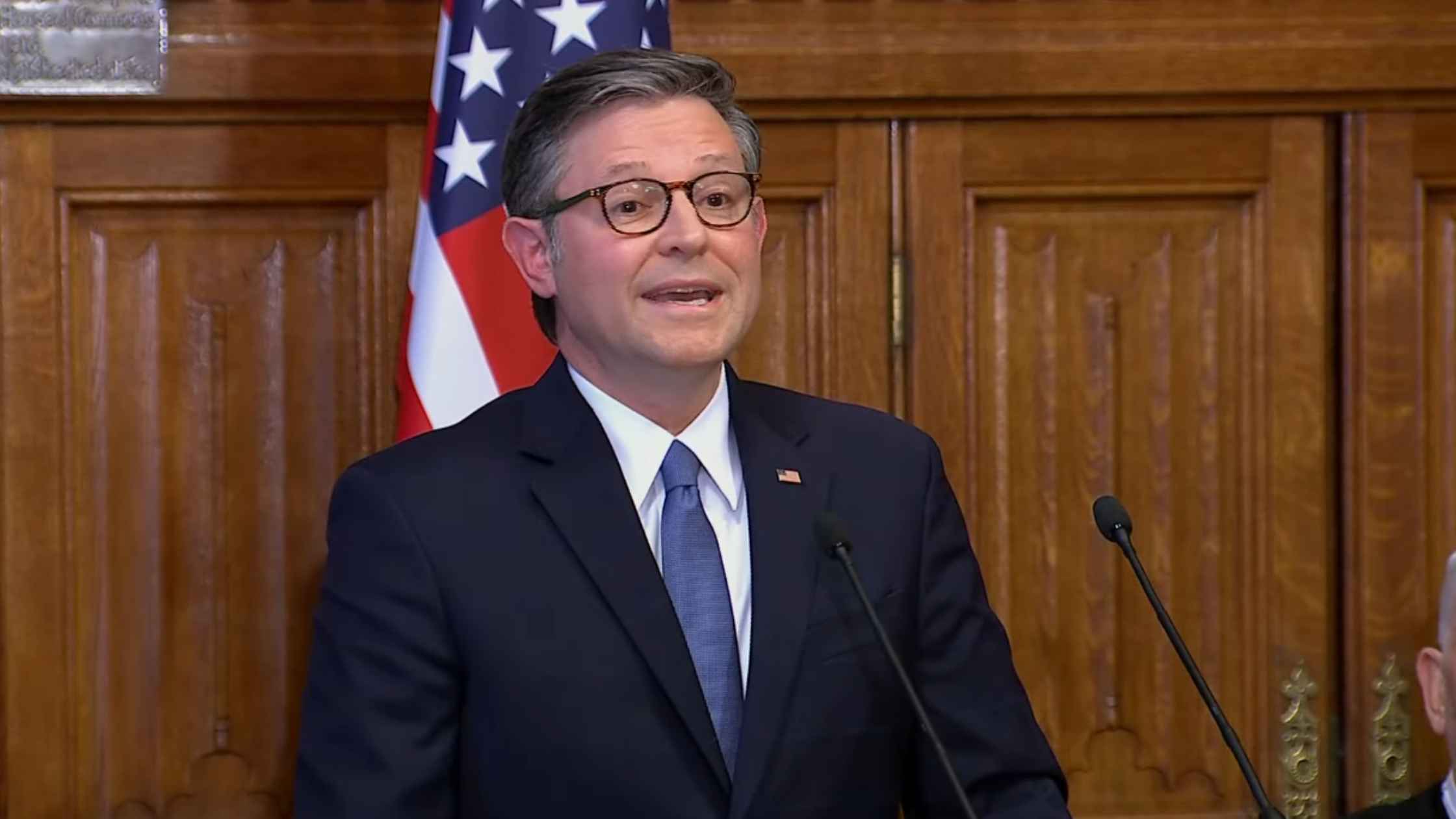
Johnson Addresses UK Lawmakers
U.S. House Speaker Mike Johnson delivers a speech in the UK Parliament in London. Read the transcript here.
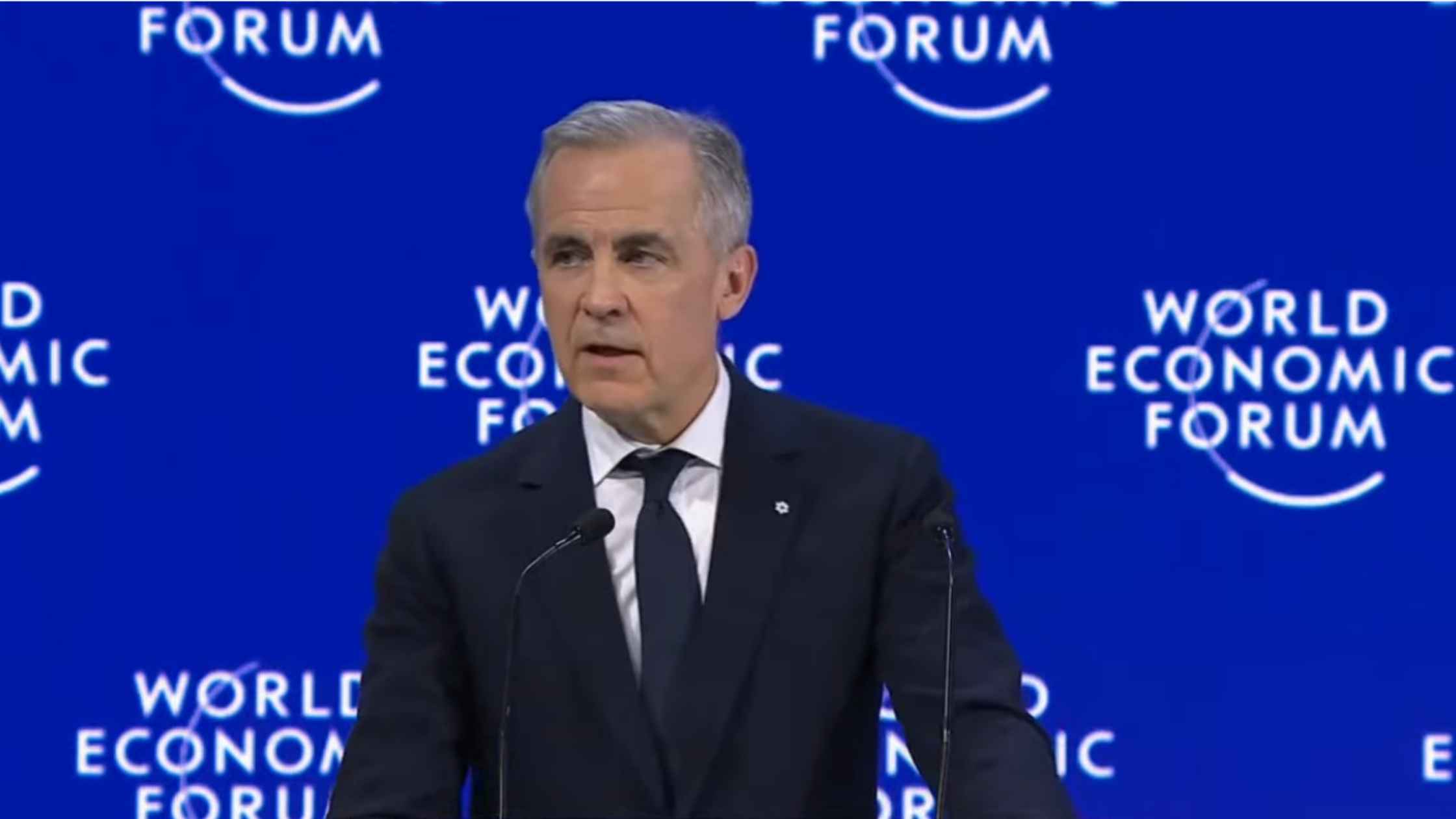
Carney at Davos
Canadian Prime Minister Mark Carney delivers a special address at the 2026 World Economic Forum in Davos. Read the transcript here.
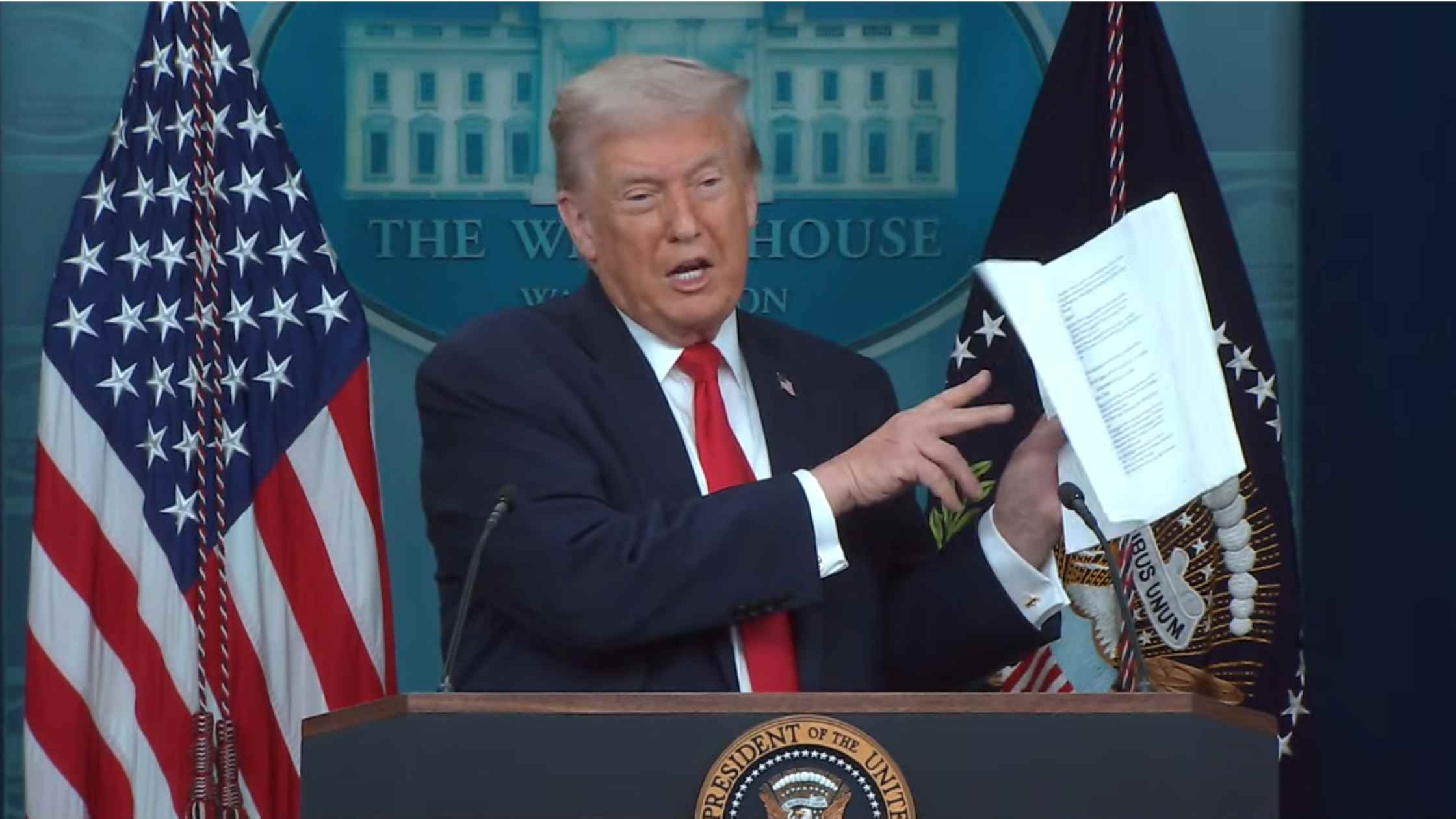
Donald Trump White House Press Briefing on 1/20/26
Donald Trump holds the White House Press Briefing for 1/20/26. Read the transcript here.
Subscribe to The Rev Blog
Sign up to get Rev content delivered straight to your inbox.








