Rev’s Transcript Library
Explore our extensive collection of free transcripts from political figures and public events. Journalists, students, researchers, and the general public can explore transcripts of speeches, debates, congressional hearings, press conferences, interviews, podcasts, and more.

Zelenskyy at WEF
Ukrainian President Volodymyr Zelenskyy delivers a special address at the 2026 World Economic Forum in Davos, Switzerland. Read the transcript here.
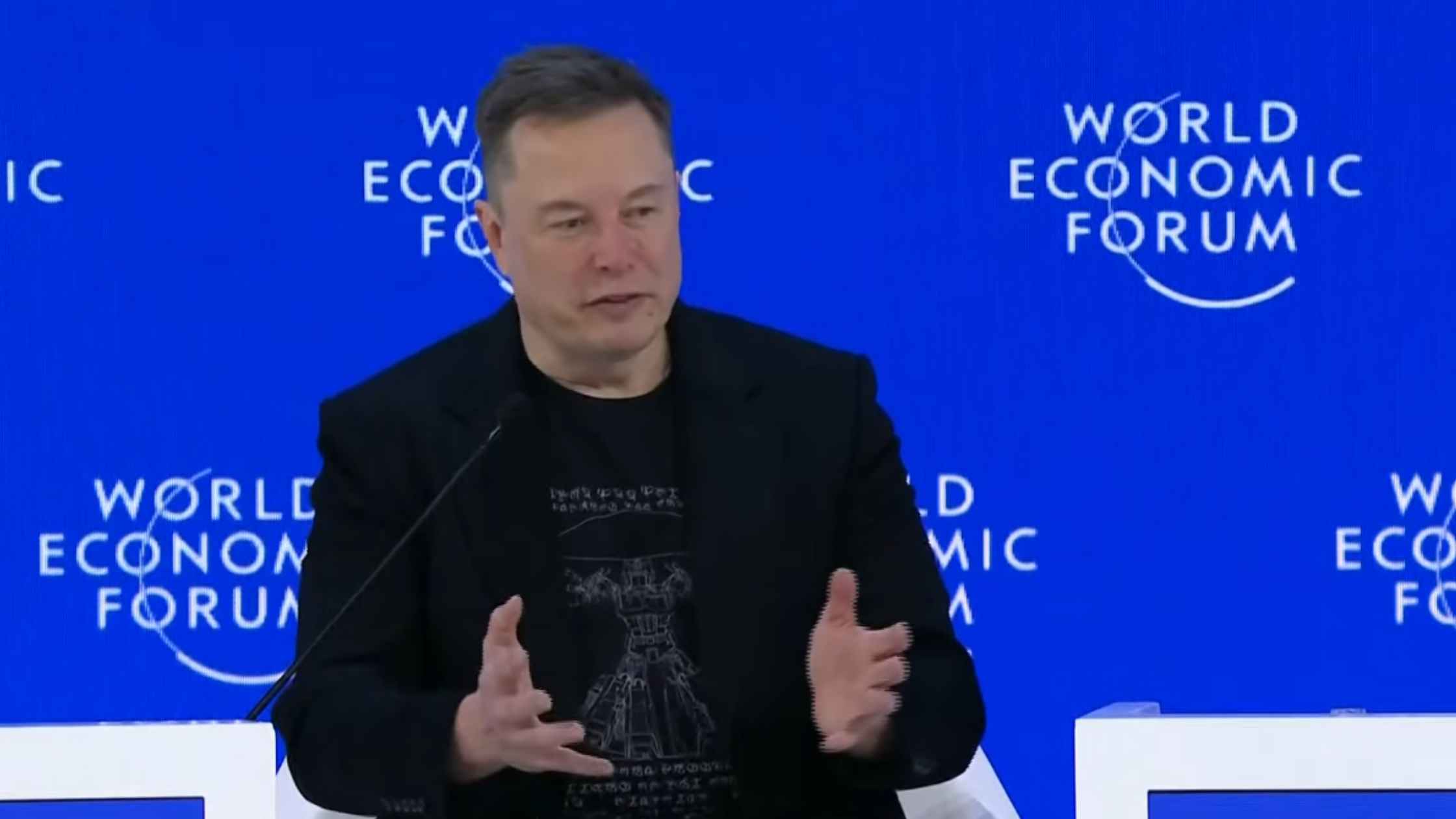
Musk Speaks at WEF
Tesla CEO, SpaceX chief engineer, and xAI CTO Elon Musk participates in a discussion at the 2026 World Economic Forum in Davos. Read the transcript here.

Minneapolis Mayor Press Conference 1/24/25
Minneapolis Mayor Jacob Frey holds a Press conference following a deadly shooting. Read the transcript here.

Border Patrol Press Conference on 1/24/26
Border Patrol chief Greg Bovino holds a news conference on immigration operations in Minneapolis. Read the transcript here.
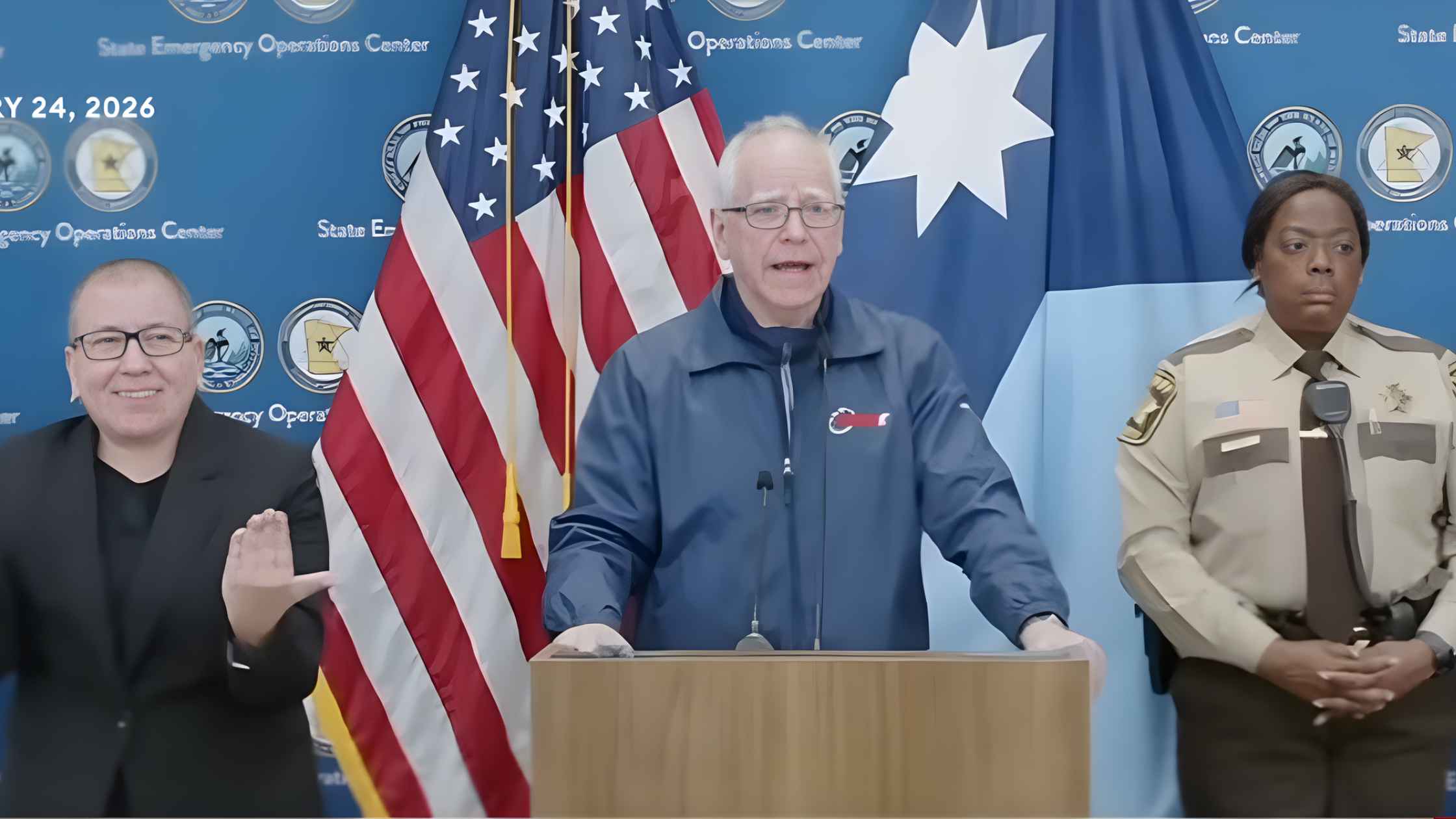
Walz Press Conference after New Shooting
Minnesota Governor Tim Walz holds a press conference after the shooting in Minneapolis on 1/24/26. Read the transcript here.
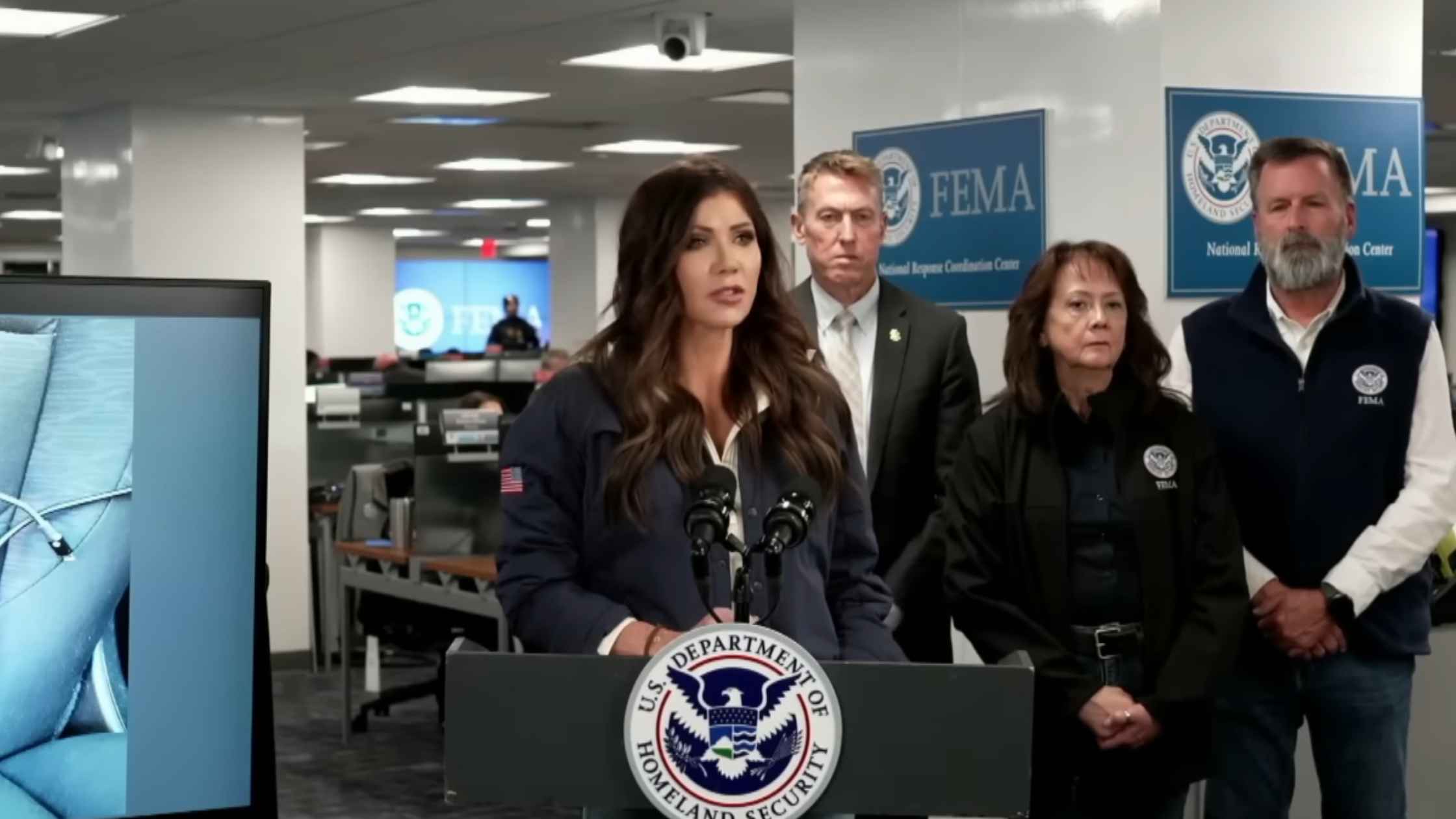
DHS Press Briefing 1/24/25
Kristi Noem holds a press conference after a federal immigration officer shot and killed a man Saturday in Minneapolis. Read the transcript here.

2026 Oscar Nominations
Danielle Brooks and Lewis Pullman announce the nominations for the 2026 Oscars.
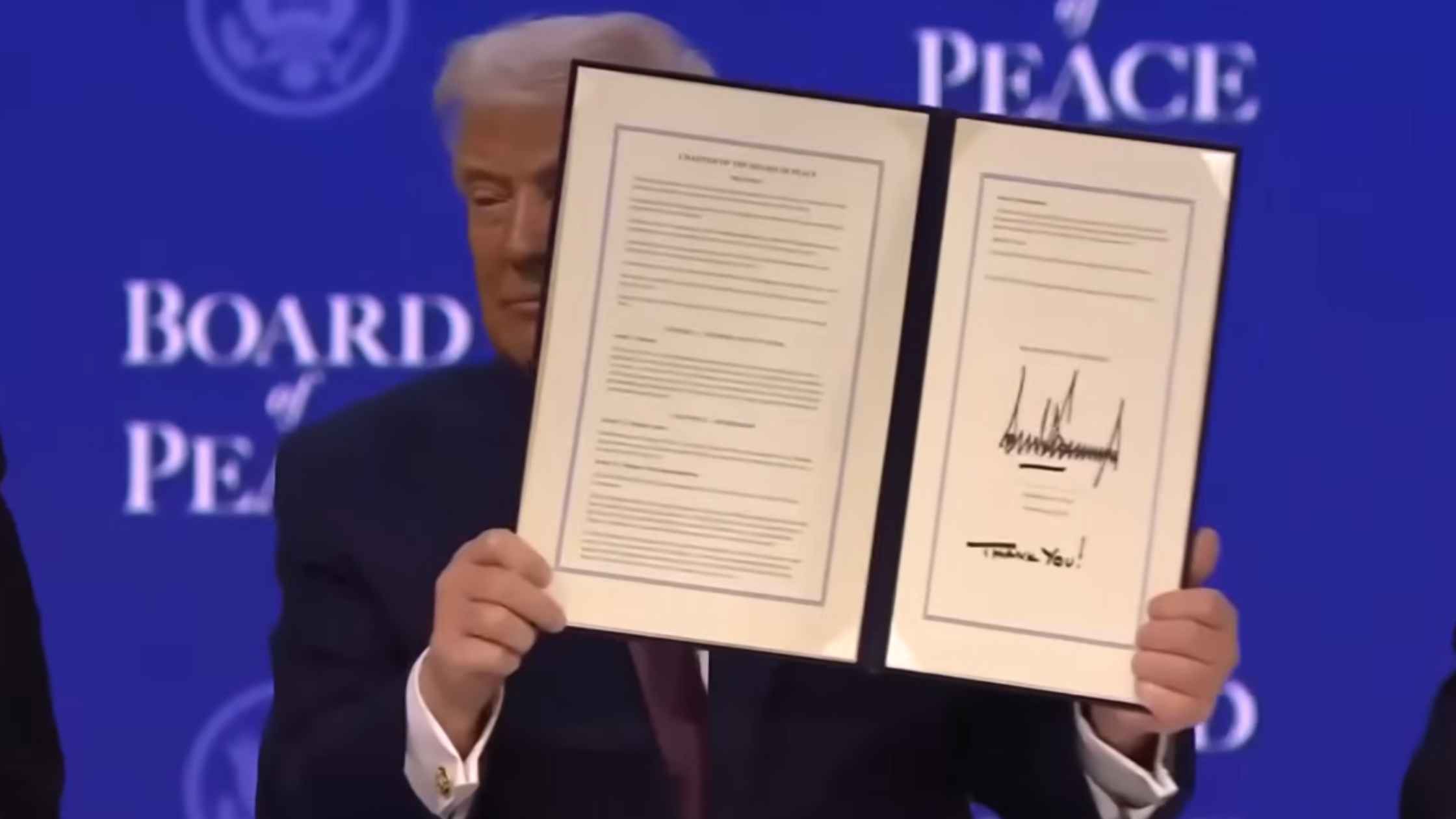
Board of Peace
U.S. President Donald Trump takes part in the Board of Peace charter announcement. Read the transcript here.
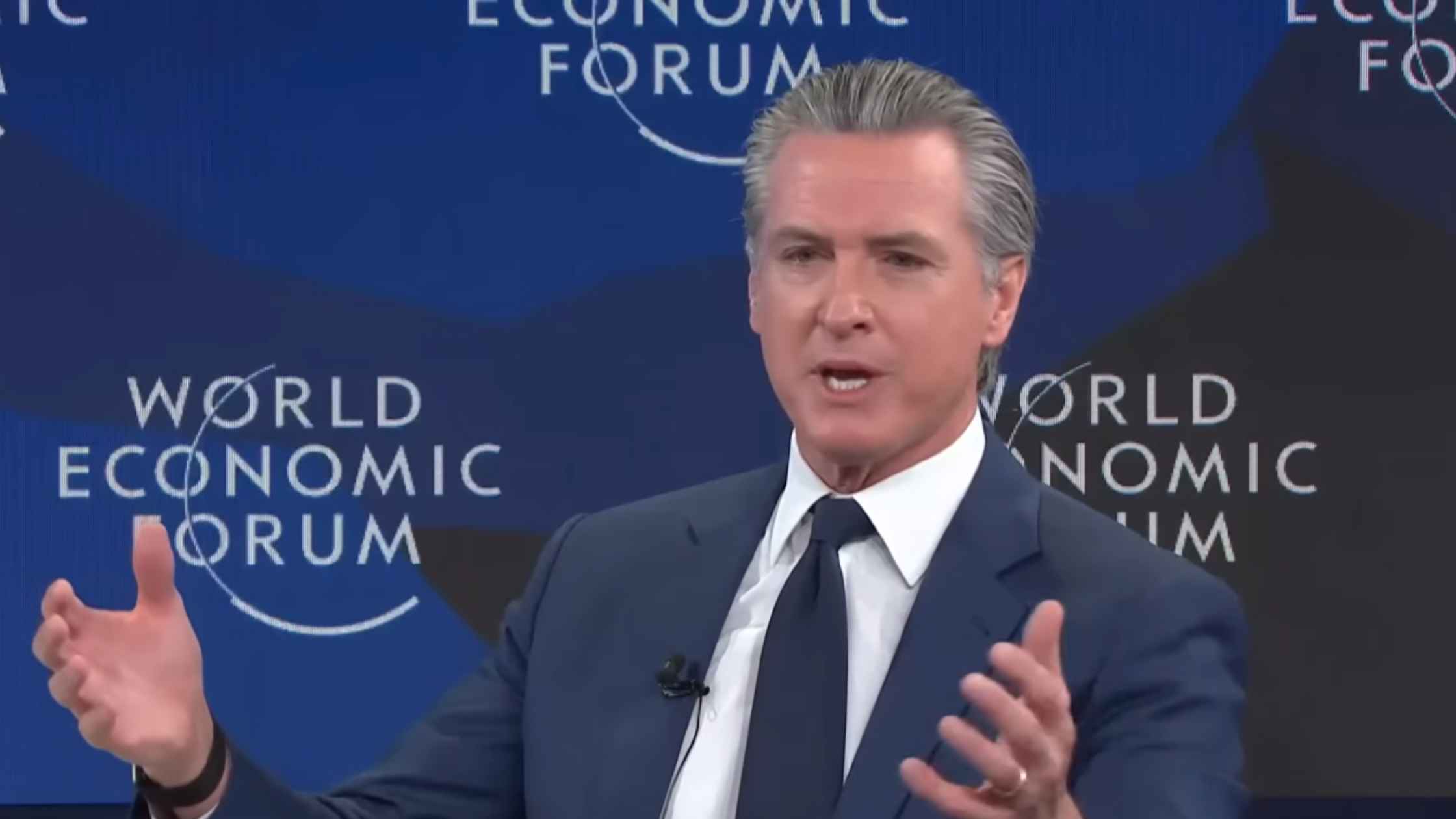
Newsom at Davos
California Governor Gavin Newsom speaks at the World Economic Forum in Davos. Read the transcript here.
Subscribe to The Rev Blog
Sign up to get Rev content delivered straight to your inbox.








