Rev’s Transcript Library
Explore our extensive collection of free transcripts from political figures and public events. Journalists, students, researchers, and the general public can explore transcripts of speeches, debates, congressional hearings, press conferences, interviews, podcasts, and more.

Senate Hearing on Rogue Judges
Ted Cruz leads the Senate Judiciary Committee Hearing on 'Holding Rogue Judges Accountable'. Read the transcript here.

Walz Addresses Minnesota ICE Shooting
Minnesota Governor Tim Walz took questions from reporters after an ICE agent shot and killed a woman in Minneapolis. Read the transcript here.
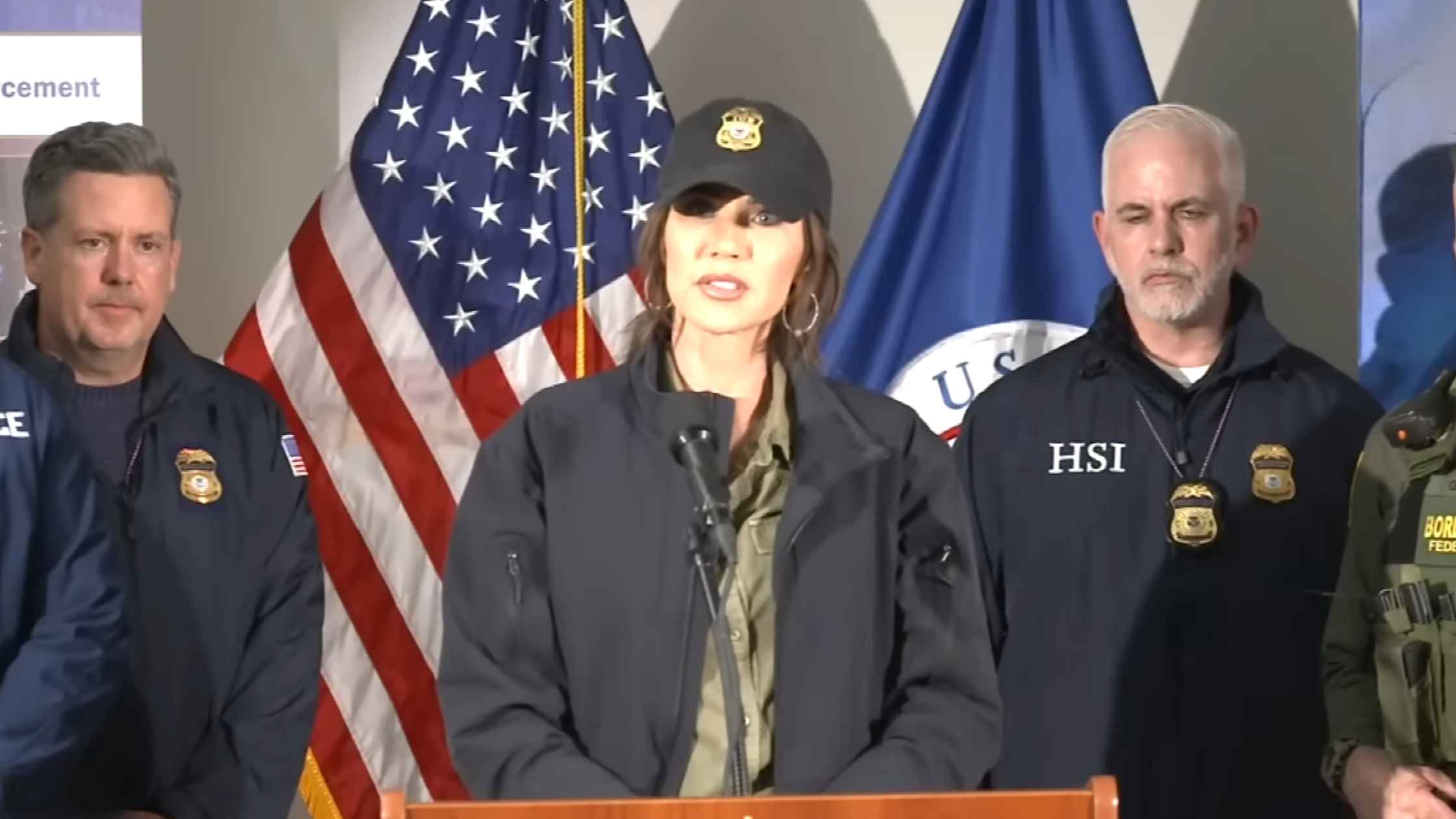
Noem Speaks on Minnesota ICE Shooting
DHS Secretary Kristi Noem holds a news conference in Minneapolis after the fatal ICE shooting of a woman. Read the transcript here.

Minnesota ICE Shooting Press Conference
Minneapolis Mayor Jacob Frey and Police Chief Brian O'Hara hold a press conference to address the fatal shooting of a woman by ICE. Read the transcript here.
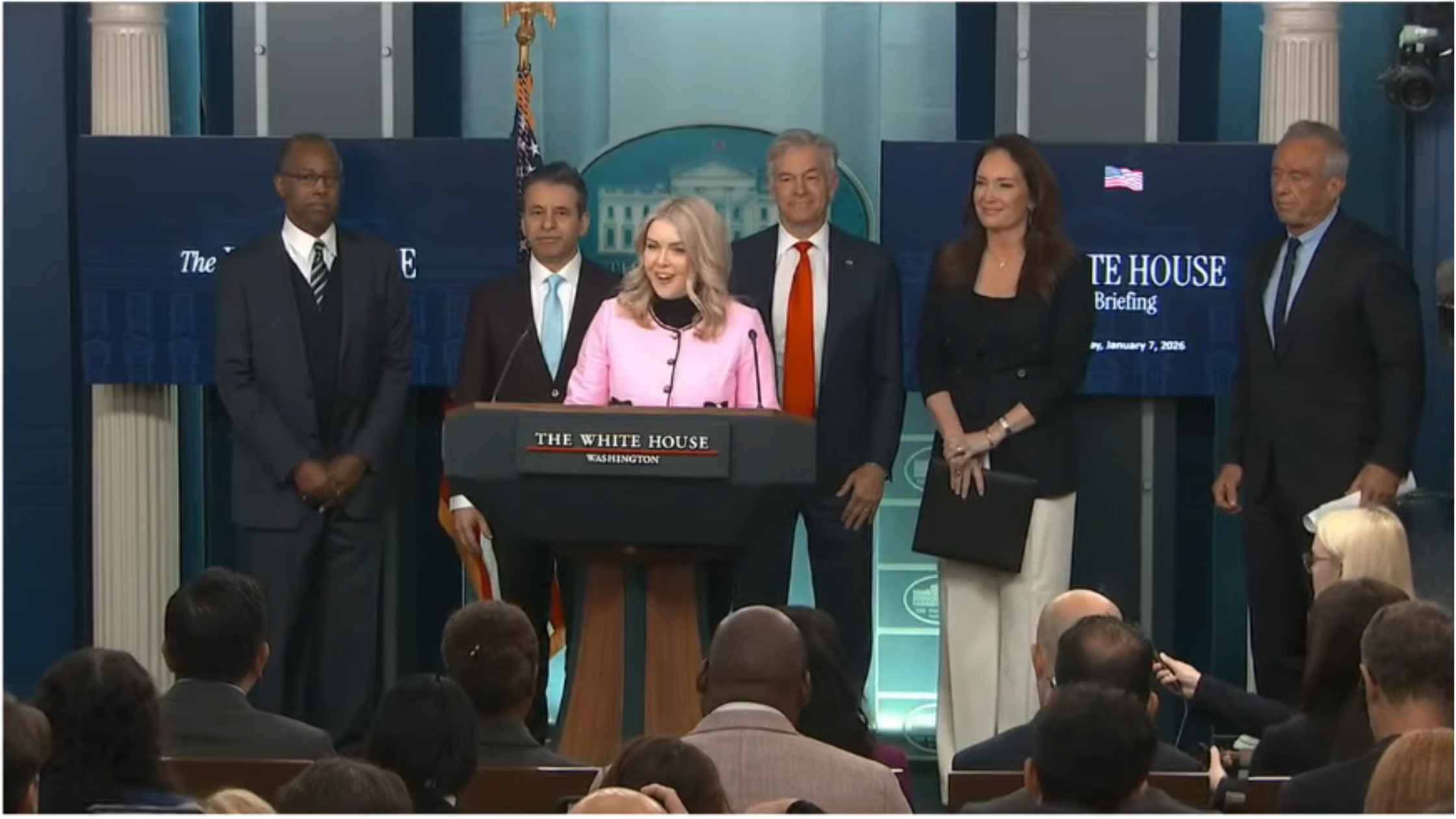
Karoline Leavitt White House Press Briefing on 1/07/26
Karoline Leavitt holds the White House Press Briefing for 1/07/26. Read the transcript here.

Coalition of the Willing
Emmanuel Macron, Keir Starmer, Volodymyr Zelenskyy, and Friedrich Merz hold a joint news conference on Ukrainian security. Read the transcript here.

January 6th Anniversery Panel
Hakeem Jeffries, select committee members, and guests hold a panel on the 5th anniversary of the Jan. 6th attack on the Capitol. Read the transcript here.
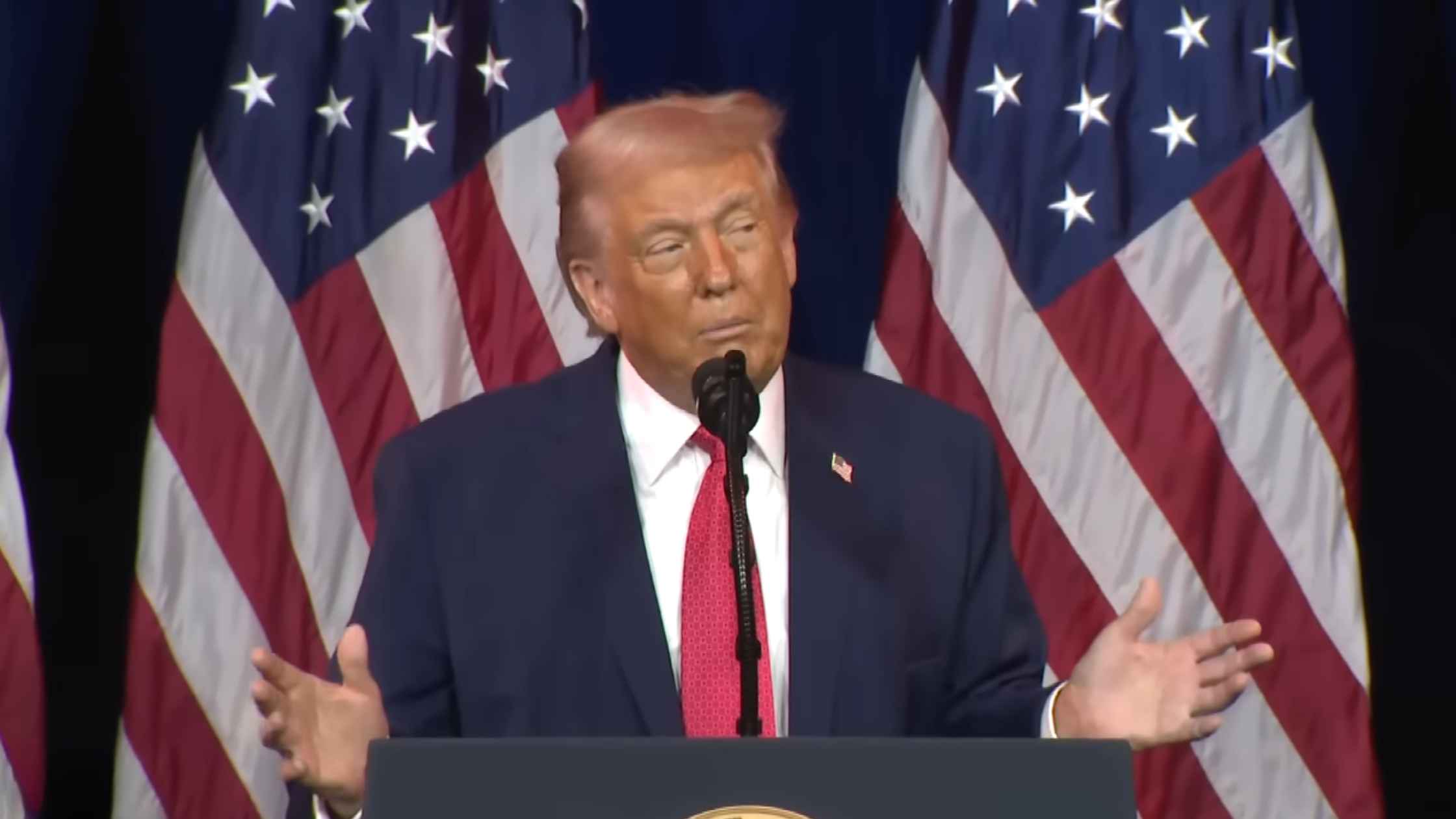
House GOP Retreat
Donald Trump speaks at a House GOP retreat at the Kennedy Center in Washington, D.C. Read the transcript here.

U.K. Foreign Secretary Makes Statement on Venezuela
U.K. Foreign Secretary Yvette Cooper makes a statement on Venezuela following the surprise U.S. military capture of President Nicolas Maduro. Read the transcript here.
Subscribe to The Rev Blog
Sign up to get Rev content delivered straight to your inbox.








